The knee joint is a pivotal complex in human movement, anatomy, and physiology, being instrumental in enabling a wide range of motions while supporting significant loads. Appreciating the knee's anatomy and biomechanics is essential for medical students, clinicians, and surgeons to diagnose, treat, and manage the vast array of conditions that can affect this joint. This chapter aims to lay the foundational knowledge required to delve deeper into the intricacies of the knee's structure and function.
The knee is not only the largest joint in the human body but also one of the most crucial for performing daily activities and high-demand athletic endeavors. Its unique anatomy allows for flexion, extension, and slight rotational movements necessary for walking, running, sitting, and standing. The knee's functionality stems from its intricate design, including bones, cartilages, ligaments, tendons, and muscles working in unison. However, its complexity and the high mechanical demands placed upon it render the knee susceptible to injuries and degenerative diseases, making an understanding of its anatomy and biomechanics paramount for medical professionals.
The knee's anatomy is a marvel of natural design, allowing it to meet the various demands placed upon it. The knee is a hinge joint with some rotational capabilities, primarily involving three bones: the femur, the tibia, and the patella, with the fibula playing no direct role in the knee joint itself. The articular surfaces of these bones are covered with hyaline cartilage, providing a smooth, low-friction surface for joint movements.
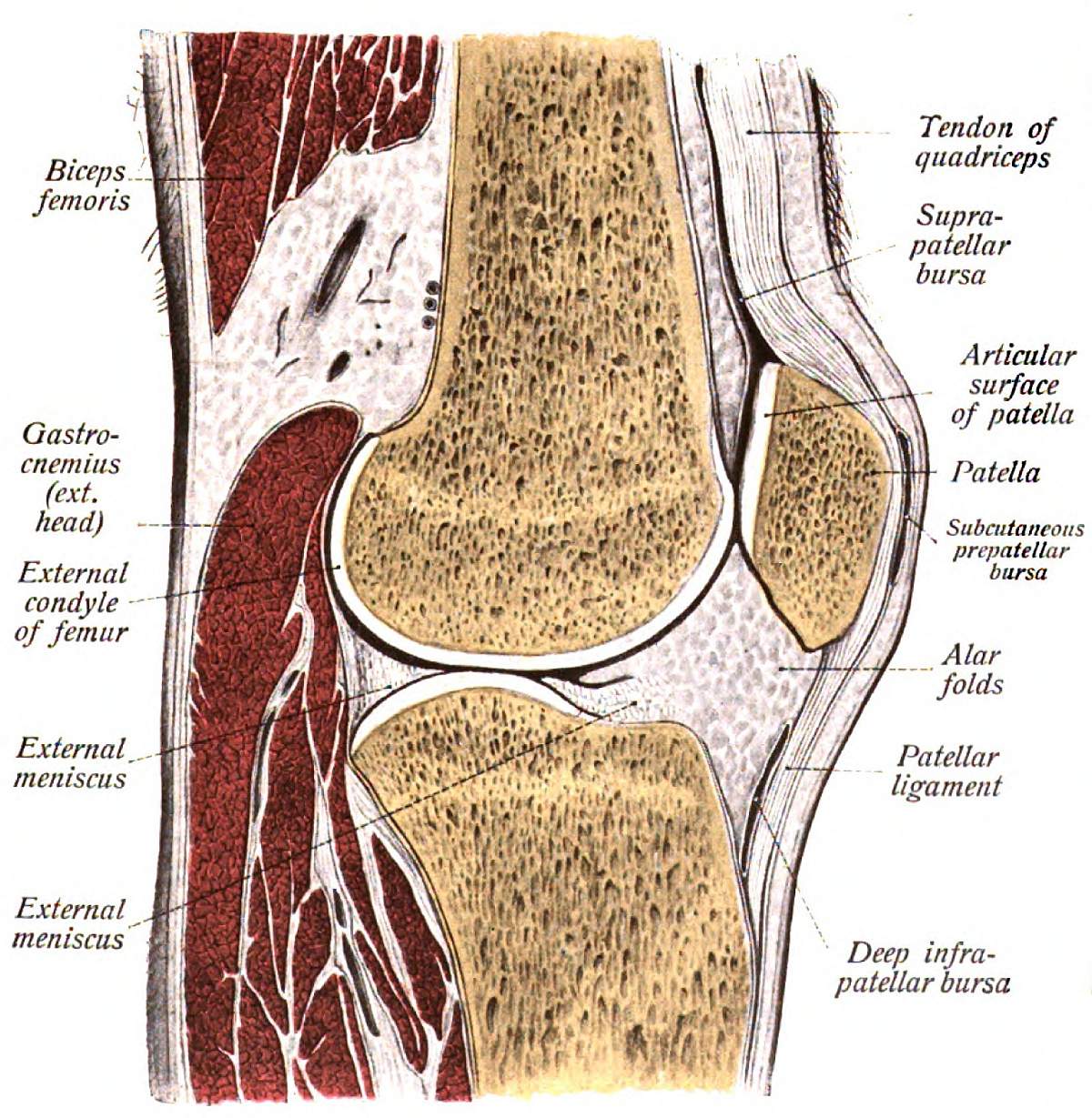
Bones and Cartilages: The femur terminates in two condyles that articulate with the flat tibial plateau and the patella, forming the main articulations of the knee. The patella, or kneecap, is a sesamoid bone embedded in the quadriceps tendon, enhancing the mechanical efficiency of knee extension. The cartilaginous structures, including the menisci, serve as shock absorbers and facilitate the complex gliding and rotational movements of the knee.
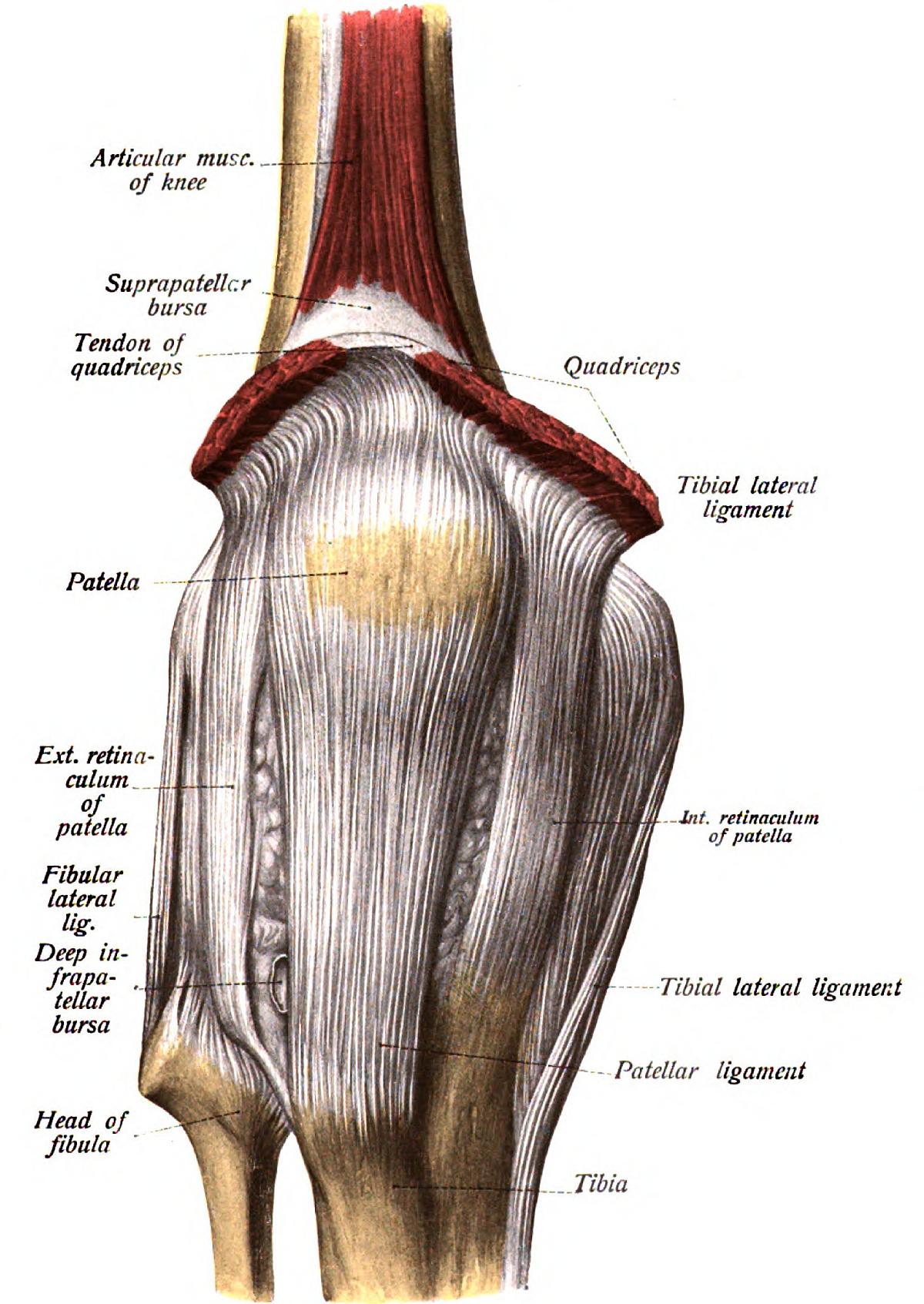
Ligaments and Tendons: Ligamentous structures, including the anterior and posterior cruciate ligaments (ACL and PCL), and the medial and lateral collateral ligaments (MCL and LCL), provide stability by preventing excessive movements. The cruciate ligaments control the anterior and posterior sliding of the tibia under the femur, while the collateral ligaments resist varus and valgus forces. The quadriceps tendon, incorporating the patella, and the patellar tendon, connect the muscle to the bone, allowing for knee extension.
Menisci and Bursae: The medial and lateral menisci are fibrocartilaginous pads that deepen the tibial plateau, aiding in load distribution and shock absorption. Several bursae, fluid-filled sacs, are strategically located around the knee to reduce friction between moving parts.
Musculature: The muscles surrounding the knee, chiefly the quadriceps, hamstrings, and the muscles of the calf, play critical roles in movement and stabilization. The quadriceps, at the front of the thigh, are key to knee extension, while the hamstrings, located at the back of the thigh, facilitate knee flexion.
Joint Capsule and Synovial Membrane: Encasing the knee is the joint capsule, lined with the synovial membrane, which secretes synovial fluid to lubricate the joint. This capsule is reinforced by the fibrous membrane on the outside and the synovial membrane on the inside, contributing to the joint's stability.
Understanding the knee's anatomy and biomechanics equips medical students and professionals with the knowledge to assess knee function, diagnose pathologies, and appreciate the implications of injuries and diseases affecting this essential joint.
The patella, often regarded as the kneecap, plays a pivotal role in the biomechanics and overall function of the knee joint. It is a unique bone in several aspects, not least because it is the largest sesamoid bone in the human body and it is embedded within the quadriceps tendon. This chapter aims to dissect the intricacies of the patella's anatomy, its functional significance, and the pathologies that might afflict it, focusing on patellar fractures.
xxxThe patella's anatomy constitutes a fascinating study, offering insight into its function and the reasons behind its susceptibility to specific injuries.
The patella is a short, flattened bone with a somewhat triangular shape when viewed from the front. It presents two noteworthy faces: the anterior and the articular (or posterior). The anterior face is convex and rough, providing attachment points for various connective tissues. Meanwhile, the articular face interacts intimately with the femur's patellar surface, featuring a vertical crest that divides it into lateral and medial facets. The lateral facet, typically more extensive, plays a significant role in articulation with the femur.
The patella's structure also includes a base and an apex (or peak). The base is oriented superiorly; it is the broader, upper part of the patella where the powerful quadriceps tendon inserts. The apex points inferiorly, giving attachment to the patellar ligament, which extends down to the tibia. The positioning and orientation of these elements are crucial for the patella's functionality during knee movements.
The anterior face's rough texture is due to its role in tendon attachment, which necessitates a surface conducive to strong connective tissue adherence. Conversely, the articular face is smooth, covered with hyaline cartilage, facilitating a low-friction interface with the femur. This posterior face is critical for dissipating the forces exerted on the knee joint, effectively protecting both the patella and the femur from excessive wear.
The patella is integral to the knee joint's functionality, primarily acting as a fulcrum to increase the quadriceps muscle's leverage. By converting the muscular force into a more efficient linear vector, it enhances the knee's extension capability. Additionally, it protects the anterior aspect of the knee joint, distributing stress and reducing friction during movement. The patella also contributes to the stabilization of the knee, aiding in the alignment and tracking of the quadriceps tendon over the femur.
Despite its robustness and critical role in knee mechanics, the patella is not immune to injury. One of the most common issues it faces is the occurrence of fractures.
Patellar fractures are significant clinical problems that can severely impact knee function. They usually result from direct trauma to the knee or, less commonly, from violent contraction of the quadriceps muscle, which can cause the patella to crack under the stress. These fractures can be classified based on their morphology (e.g., transverse, comminuted, vertical) and whether the fracture is displaced or non-displaced. The treatment approach varies, ranging from non-operative management involving immobilization for non-displaced fractures, to surgical intervention for displaced fractures to restore the articular surface and functional integrity of the extensor mechanism.
In summary, understanding the patella's anatomy and function is crucial for diagnosing and managing injuries effectively. The patella's unique structure and the critical role it plays in knee biomechanics make it an indispensable area of study for medical students and professionals alike, with an eye towards optimizing patient outcomes in patellar pathologies.
The knee joint, known as the articulatio genus, is a pivotal structure in human locomotion, representing one of the most complex and largest joints in the human body. Its design enables it to withstand significant mechanical stress while providing flexibility and stability. This chapter delves into the anatomical composition and biomechanics of the knee joint, providing a comprehensive understanding crucial for medical students.
Understanding the knee joint requires a thorough examination of its components. The knee is essentially a hinge joint with the capability to perform slight rotation and lateral movements. The main anatomical structures involved include the femoral condyles, the tibial plateau, and the patella. Let's explore these components in detail.
The femoral condyles are integral to the knee's biomechanics, forming the upper portion of the joint. These two convex surfaces located on the distal end of the femur articulate with the tibial plateau. The medial condyle, being longer and more pronounced, contributes to the knee's stability by fitting into the concavity of the tibial plateau. The lateral femoral condyle, slightly shorter and less curved, facilitates the rotational movement of the knee. Both condyles are covered with a 2-3 mm thick hyaline cartilage, reducing friction and distributing mechanical stress during knee movements.
The tibial plateau is the upper surface of the tibia that interacts with the femoral condyles. It consists of two slightly concave articular surfaces separated by the intercondylar eminence, contributing to knee stability. The articular cartilage thickness varies, being thinner at the periphery and thicker centrally, allowing for better force distribution. The articular correspondence, or the matching of surfaces between the femoral condyles and the tibial plateau, is crucial for the knee's functional integrity. The incongruence of these articular surfaces is compensated by the menisci, semi-lunar cartilages that deepen the tibial concavities, improving joint congruence and load distribution.
The biomechanics of the knee joint are governed by its anatomical structures and their interactions during movement. This section explores how these components work together to facilitate joint movement and ensure stability and protection.
The knee joint allows for two primary movements: flexion and extension. During these movements, the patella, or kneecap, slides over the femoral condyles, acting as a fulcrum that increases the leverage of the quadriceps muscle. This mechanism is essential for activities such as walking, running, and jumping. The joint's stability during these movements is ensured by a complex system of ligaments, including the cruciate and collateral ligaments, which control the forward and backward movement of the tibia in relation to the femur and provide lateral stability, respectively.
Proper alignment of the knee joint is vital for distributing loads across the articular surfaces, minimizing wear and tear, and preventing injuries. The alignment is influenced by the shape and congruence of the articular surfaces, the tension and integrity of the ligaments, and the strength and coordination of surrounding muscles. Misalignment can lead to abnormal stress distribution, leading to conditions such as osteoarthritis. The articular surfaces of the knee are designed to maximize contact area during weight-bearing activities, with the menisci playing a crucial role in evenly distributing compressive forces, thus protecting the underlying bone and cartilage from excessive stress.
In summary, the knee joint's anatomical design and its biomechanical properties allow for a remarkable range of movements while providing stability and protection against the mechanical stresses of daily activities and sports. Understanding these principles is fundamental for medical students, as it lays the groundwork for diagnosing and treating knee-related pathologies effectively.
The menisci of the knee are two crescent-shaped fibrocartilaginous structures crucial for the efficient functioning and biomechanics of the knee joint. They play a vital role in shock absorption, load distribution, and joint stability. Understanding their structure, function, and vulnerabilities is essential for medical students who will encounter various meniscal injuries in their clinical practice.
The knee joint contains two menisci: the medial and the lateral. Each meniscus sits between the femoral condyle and the tibial plateau of its respective side. The medial meniscus presents as a semilunar shape, and is broader posteriorly than anteriorly. It is firmly attached to the deep medial collateral ligament, contributing to its vulnerability to injuries. The lateral meniscus is almost circular and more mobile than the medial meniscus, due to its looser attachment to the lateral collateral ligament. Each meniscus has two surfaces: a concave superior surface that articulates with the femoral condyle, and a roughly flat inferior surface that sits on the tibial plateau. The menisci are also attached to the tibia via their anterior and posterior horns.
The menisci serve several critical functions within the knee joint. They act to distribute the body's weight more evenly across the articular surfaces of the knee, reducing the peak stress on any single point. This load distribution is crucial for preventing localized wear and tear on the cartilage. The menisci also work as shock absorbers, cushioning the knee against impacts. Additionally, by deepening the articular surface of the tibia, they contribute to the joint's stability by aiding in the prevention of excessive movement of the femur on the tibial plateau. The menisci significantly improve the congruence between the two bones, enhancing the efficiency of the knee as a hinge joint.
Meniscal injuries can range from minor tears to severe ruptures, affecting the knee's functionality and stability. They are common in athletes and can result from both acute trauma and chronic degeneration. Proper diagnosis and management of meniscal injuries are pivotal in preserving knee joint health and preventing the onset of osteoarthritis.
Meniscal tears are classified based on their appearance (horizontal, vertical, radial, complex) and location (anterior horn, body, posterior horn). Symptoms often include pain, swelling, popping, and difficulty moving the knee. The "locking" of the knee is a characteristic sign of a meniscal tear, where the knee gets stuck in one position due to a piece of the torn meniscus blocking joint movement.
Diagnosis of meniscal injuries involves a thorough patient history, physical examination, and imaging tests such as MRI, which provides a detailed view of soft tissues, including the menisci. Treatment strategies may vary from conservative management, including rest, ice, compression, and elevation (RICE), to surgical interventions like meniscectomy or meniscal repair, depending on the severity of the injury, the patient's age, and activity level.
Understanding the complex anatomy and functionality of the menisci is crucial in diagnosing, managing, and preventing injuries to these vital structures. Their role in maintaining knee stability, distributing loads, and preventing degenerative changes highlights the importance of conserving meniscal integrity whenever possible.
Ligaments and tendons play crucial roles in the functional stability and mobility of the knee joint, one of the largest and most complex joints in the human body. Understanding the anatomy, biomechanics, and potential injury mechanisms of these structures is paramount for medical students, as it lays the foundation for diagnosing and treating knee-related issues.
The patellar ligament, a critical component of the extensor mechanism of the knee, extends from the patella's apex to the tibial tuberosity. Functionally, it is the terminal portion of the quadriceps femoris tendon, with the patella embedded within it as a sesamoid bone. This anatomical arrangement enhances the quadriceps muscle's mechanical advantage, crucial for knee extension. The patellar ligament is approximately 5-6 cm in length and 2-3 cm wide, with a triangular shape. Its anterior surface is exposed, making it palpable under the skin, especially during semi-flexion of the knee. The posterior aspect is related to the infrapatellar adipose body and deep infrapatellar bursa, which facilitate smooth movement and prevent friction. An understanding of the patellar ligament's anatomy is essential when considering conditions such as patellar tendinitis or patellar ligament rupture, both common in athletes.
The complexity of the knee's posterior aspect is underscored by the presence of several ligaments that contribute to its stability and facilitate movement.
The oblique popliteal ligament, a broad fibrous band, originates from the semimembranosus tendon's expansion. It travels superiorly and laterally to attach to the lateral femoral condyle. This ligament plays a pivotal role in stabilizing the posterior aspect of the knee joint.
The arcuate popliteal ligament, characterized by its individual variability, typically forms a fibrous arch with its base at the lateral femoral condyle and spans medially beneath the oblique popliteal ligament. This structure contributes to the lateral stability of the knee and protection against hyperextension. Both these ligaments, with their complex insertions and pathways, underscore the knee's dynamic capability to withstand various forces during movement while maintaining stability.
These ligaments are fundamental to the knee's structural integrity, each playing specific roles in joint stability and movement.
The collateral ligaments, consisting of the fibular (lateral) and tibial (medial) collateral ligaments, guard against excessive lateral or medial gapping of the knee joint. The fibular collateral ligament, originating from the lateral epicondyle of the femur and inserting onto the head of the fibula, is particularly important for stabilizing the lateral knee and is taut during knee extension. The tibial collateral ligament has a broader attachment, extending from the medial epicondyle of the femur to the medial aspect of the tibia. It is intimately associated with the medial meniscus, emphasizing the interconnectedness of knee structures in maintaining joint stability.
The cruciate ligaments, comprising the anterior and posterior cruciate ligaments (ACL and PCL), function to prevent anterior and posterior displacement of the tibia relative to the femur. The ACL, originating from the anterior intercondylar area of the tibia, inserts into the lateral femoral condyle in a complex, oblique orientation. This positioning allows it to resist anterior tibial translation and rotational forces. The PCL, larger and stronger, prevents posterior displacement of the tibia and emanates from the posterior intercondylar area, attaching to the medial femoral condyle.
Cruciate ligaments are often the subject of sports-related injuries, with ACL tears being among the most common knee injuries in athletes. The mechanism frequently involves a sudden stop, change in direction, or direct impact to the front of the knee, leading to overstretching or tearing of the ligament. PCL injuries typically result from a blow to the anterior shin while the knee is bent, such as in a car accident or during sports. Understanding these mechanisms is crucial for the prevention, diagnosis, and treatment of such injuries.
The collateral ligaments, by contrast, are more frequently injured as a result of direct blows to the side of the knee, forcing the knee sideways and stretching or tearing these support structures. The medial collateral ligament is particularly vulnerable to such lateral impacts due to its exposure and broader attachment span.
In conclusion, the ligaments and tendons of the knee work in concert to provide stability, enable movement, and protect against injury. Their complex anatomy and biomechanics require a thorough understanding by medical students and professionals alike, serving as the foundation for effective diagnosis, treatment, and injury prevention strategies related to the knee joint.
The knee joint is encapsulated by a complex, fibrous, connective tissue membrane that not only encompasses the articulating bones — the femur, tibia, and patella — but also plays a crucial role in the joint's structural integrity, flexibility, and protection. The capsule is distinctive in its configuration, adapting to the contours of the knee's components, thus ensuring optimal function. It originates from the margin of the articular surfaces of the involved bones, extending from the femoral condyles down to the tibial plateau, enveloping the patella anteriorly while excluding the fibula.
This capsular structure is divided into two integral layers: a fibrous outer layer and an inner synovial layer. The fibrous outer layer is characterized by its dense connective tissue, which contains longitudinally, transversely, and obliquely oriented collagen fibers. These fibers confer strength and flexibility, allowing the knee joint to withstand the mechanical stresses imposed upon it during movement. The regions of this fibrous layer vary in thickness, with reinforcement occurring posteriorly through the incorporation of additional capsular and extracapsular ligamentous structures, such as the oblique popliteal ligament, which enhances the joint's stability.
The knee capsule's orifices, specifically the large anterior aperture for the patella and the posterior aperture at the intercondylar notch, are functionally significant. They accommodate the joint's articulating surfaces and facilitate the extension of the synovial membrane to the interior aspects of the joint. Smaller orifices present within the capsule serve as conduits for vessels and nerves, and for the protrusion of synovial fringes.
The synovial membrane is a specialized connective tissue lining the interior of the joint capsule, excluding the articular cartilages and the intra-articular ligaments. This thin, delicate membrane plays a pivotal role in the production of synovial fluid, a clear, viscous secretion that lubricates the joint surfaces, reducing friction and wear between them. This lubrication mechanism is essential for the smooth movement of the knee and for nourishing the articular cartilages, thus preserving joint health.
The synovial membrane extends beyond the main cavity of the knee joint, forming several bursae — sac-like structures filled with synovial fluid. These bursae are strategically located to minimize friction between the joint capsule, tendons, muscles, and overlying skin. A prominent example is the suprapatellar bursa, located above the patella, which facilitates the sliding of the quadriceps femoris muscle over the distal end of the femur. Other significant bursae include the subpopliteal recess and the bursae associated with the pes anserinus, serving essential roles in cushioning and facilitating movement.
The synovial membrane's extensive surface area and its role in fluid production make it susceptible to infections and inflammatory conditions. Infections within the joint capsule (septic arthritis) can lead to the rapid accumulation of pus within the joint, necessitating prompt medical intervention to prevent cartilage damage and preserve joint function. The synovial membrane can also be involved in systemic inflammatory conditions, such as rheumatoid arthritis, where immune-mediated processes lead to synovial hypertrophy and joint effusion, resulting in pain, swelling, and decreased mobility of the knee.
In managing diseases affecting the synovial membrane and the knee capsule, clinicians must adopt a comprehensive approach, considering both the infectious and autoimmune etiologies. Therapeutic strategies may involve pharmacological interventions to manage inflammation and infection, surgical interventions for drainage and debridement, and rehabilitative measures to restore function. Understanding the intricate relations within the capsular structure and synovial membrane is essential for diagnosing knee pathologies accurately and formulating effective treatment plans.
In presenting these concepts from the perspective of a medical educator, the above discussion elucidates the critical features and functions of the knee capsule and synovial membrane, integrating anatomical and physiological knowledge to lay a foundation for understanding knee joint pathologies and their management.
Understanding the biomechanics and movement of the knee joint is essential for medical professionals to diagnose and treat disorders effectively. This chapter delves into the mechanics of knee flexion and extension, rotational movements, and inclinations, providing a comprehensive overview for medical students.
The knee joint, being the largest in the human body, is complex and allows for significant movements such as flexion and extension. These movements are vital for basic activities like walking, running, and jumping.
The knee operates under lever mechanics principles, specifically, a third-class lever system during flexion and extension. This means that the effort (force applied by muscles) is between the fulcrum (the knee joint) and the load (the weight of the body part being moved). In the case of knee extension, the quadriceps muscle exerts force to straighten the leg, overcoming the resistance provided by the weight of the lower leg and any external load. During this process, the patella acts as a sesamoid bone within the quadriceps tendon, increasing the mechanical advantage by changing the direction of the applied force and improving the efficiency of the knee joint during extension.
The primary muscle group involved in knee extension is the quadriceps femoris, which includes four muscles: the vastus lateralis, vastus medialis, vastus intermedius, and the rectus femoris. These muscles work together to extend the knee. The quadriceps' tendon inserts into the patella, and from there, the patellar ligament attaches it to the tibial tuberosity, completing the extensor mechanism.
Flexion, on the other hand, is mainly facilitated by the hamstrings, which are three muscles located at the back of the thigh: the biceps femoris, semimembranosus, and semitendinosus. The gastrocnemius muscle also aids in knee flexion, especially when the foot is dorsiflexed. Flexion movement is characterized by the lower leg moving towards the posterior part of the thigh, with the tibiofemoral joint allowing this motion around a transverse axis.
Apart from flexion and extension, the knee joint allows for lesser degrees of rotational and tilting movements, which are essential for the fine adjustments in body positioning and balance.
Rotational movements at the knee are categorized into medial (internal) and lateral (external) rotations and occur mainly when the knee is in a partially flexed position. This is because the collateral ligaments, which are taut during extension, relax during flexion, allowing for a greater range of rotational movement. The cruciate ligaments play a crucial role in providing rotational stability, with the anterior cruciate ligament limiting excessive internal rotation and the posterior cruciate ligament restraining excessive external rotation. Muscles that contribute to knee rotation include the femoral biceps and the medial head of the gastrocnemius for outward rotation, and the semimembranosus, semitendinosus, sartorius, popliteus, and gracilis for inward rotation.
Lateral and medial tilting of the knee is a passive movement that occurs due to the varying tension in the collateral and cruciate ligaments during knee flexion and extension. These tilting movements are of small amplitude and play a role in the fine-tuning of leg alignment during dynamic activities. The structure and function of the intra-articular menisci are critical in this context, as they contribute to the congruency and stability of the knee joint by improving the fit between the femoral condyles and tibial plateaus, facilitating the efficient transmission of mechanical forces.
In conclusion, the biomechanics of knee movements involve complex interactions between bones, muscles, ligaments, and cartilaginous structures. Understanding these interactions enables medical professionals to grasp the underlying principles governing knee function and is fundamental in diagnosing, managing, and treating knee pathologies effectively.
The patella, commonly known as the kneecap, is not just a passive bone within the knee joint; it plays a crucial role in the biomechanics of knee dynamics. Understanding its movement and stability is essential for comprehending knee function and addressing pathologies related to this complex joint. This chapter delves into the nuances of patellar movement, stability, and patellofemoral contact throughout the knee's range of motion.
The patella serves to increase the leverage of the quadriceps muscle tendon, thus enhancing the efficiency of knee extension. Its stability and movement are inherently linked to several anatomic structures, including the patellar ligament, the quadriceps tendon, and the surrounding retinacula and fascial layers.
The patella glides over the femoral condyles in a controlled manner as the knee flexes and extends. During the initial phases of flexion, the patella contacts the femoral condyles primarily through its lower third. As flexion progresses to 45°, contact shifts to the middle third, and beyond 60° of flexion, the upper third of the patella engages the femoral condyles. This sequential engagement ensures optimal load distribution and minimizes stress on any single area, thereby protecting the articular cartilage surfaces. The sliding mechanism of the patella is crucial for the knee's biomechanical efficiency, allowing for smooth transitions between flexion and extension movements.
The patella is connected to the femur not only through the quadriceps tendon but also through fibrous structures known as patellar wings. These wings, coupled with the medial and lateral patellar retinacula, form a stabilizing apparatus that guides the patella during its sliding movements. The medial and lateral retinacula are reinforced by vertical fibers that attach to the edges of the patella and the underlying tibial condyle, ensuring that the patella remains aligned within its physiological path. This alignment is critical to prevent lateral dislocation of the patella and to distribute forces evenly across the patellofemoral joint.
The contact area between the patella and the femoral condyles varies as the knee moves through its range of motion. This dynamic relationship plays a key role in distributing forces across the joint and in the biomechanical function of the knee.
During extension, the patella primarily contacts the femur at its distal pole, near the intercondylar groove. As the knee flexes, the contact area shifts upward along the patella's articular surface. This migration is essential for distributing compressive forces over a larger area, reducing stress on any single point.
The patellofemoral joint faces the highest loads during the last degrees of extension and the initial degrees of flexion. Here, the quadriceps muscle exerts significant force, pulling the patella into the femoral groove and securing it in place against the femoral condyles. The shape and contour of the patella and the femoral groove play pivotal roles in this locking mechanism, ensuring stability and efficient force transmission.
The thickness of the cartilage on the posterior surface of the patella is variable, being thinner at the periphery and thicker centrally. This differential thickness accommodates the changing contact points and forces experienced by the patella through knee movement, providing a cushion that absorbs and distributes loads.
In summary, the patella is central to knee dynamics, acting as a critical lever that enhances the efficiency of the extensor mechanism and distributing forces to protect joint surfaces. Its movement, stability, and contact with the femoral condyles through various ranges of motion illuminate the intricate biomechanics at play within the knee joint. Understanding these principles is essential for medical students as they prepare to diagnose and manage conditions of the knee.
The knee joint, being the largest and one of the most complex joints in the human body, is susceptible to a variety of pathologies. Among these, ligament injuries, meniscal tears, and bursitis represent some of the most common and clinically significant conditions affecting the knee. Understanding the detailed anatomy and biomechanics of the knee is a prerequisite for grasping the nuances of these pathologies. In this chapter, we delve into the medical intricacies of these conditions, establishing a foundation for diagnosis, management, and treatment strategies.
The knee joint is stabilized by a complex array of ligaments, including the cruciate (anterior and posterior) and collateral (tibial and fibular) ligaments. These ligaments are essential for the joint's stability and function, restraining excessive movements and aligning the joint during motion. Injuries to these ligaments are not only common in athletic populations but also occur in general populations due to trauma, accidents, or degenerative changes.
Cruciate Ligament Injuries: The anterior and posterior cruciate ligaments are critical for anterior-posterior stability of the knee. The anterior cruciate ligament (ACL) is more commonly injured than the posterior cruciate ligament (PCL) due to its role in preventing anterior translation of the tibia relative to the femur. ACL injuries often occur during sports through mechanisms such as sudden deceleration, hyperextension, or direct impact. PCL injuries, while less common, typically result from a direct force to the front of the tibia with the knee flexed, such as in a car accident. Clinically, cruciate ligament injuries present with pain, swelling, instability, and a decreased range of motion. The diagnosis is confirmed through physical examination maneuvers like the Lachman test for ACL injuries and imaging studies, such as MRI.
Collateral Ligament Injuries: The medial (tibial) and lateral (fibular) collateral ligaments provide medial and lateral stability to the knee. Injuries to these ligaments often result from a force that pushes the knee sideways—medial injuries from a force to the outer knee and lateral injuries from a force to the inner knee. Patients may report pain at the sides of the knee, swelling, and instability in the frontal plane. Diagnosis often involves stress testing of the knee and imaging studies.
The menisci are two crescent-shaped fibrocartilages between the femur and tibia that act as shock absorbers and stabilizers within the knee joint. Meniscal tears can result from both acute trauma and degenerative processes. Acute meniscal injuries often occur in combination with ligament injuries, especially ACL tears, during twisting or shearing forces on the knee. Degenerative tears are more common in older adults due to the wear and tear of the knee joint over time. Symptoms include pain, swelling, catching, and locking of the knee. Diagnostic approaches include clinical examination with maneuvers like McMurray's test and imaging, particularly MRI, which offers detailed images of soft tissues. Treatment can range from conservative management with physical therapy to surgical interventions such as meniscectomy or meniscus repair, depending on the severity and type of the tear.
The knee joint contains several bursae, which are fluid-filled sacs that reduce friction between tissues. Bursitis occurs when these bursae become inflamed, typically due to repetitive movements, prolonged pressure, or direct trauma. The most common types affecting the knee are prepatellar bursitis, often seen in individuals who kneel frequently, and pes anserine bursitis, located on the inner side of the knee. Symptoms of bursitis include localized pain, swelling, and tenderness. In some cases, the inflammation can become septic, requiring antibiotic therapy. Conservative treatment generally involves rest, ice, and anti-inflammatory medications. In refractory or septic cases, aspiration or surgical removal of the bursa may be necessary.
Understanding the detailed mechanisms of these pathologies is pivotal for medical students and practitioners alike. It not only aids in accurate diagnosis and treatment but also in educating patients about the risk factors and preventive measures to avoid such injuries and maintain knee health.
Conservative treatment options for knee injuries offer non-surgical methods aimed at alleviating symptoms, promoting healing, and improving knee function. These treatments are the first line of defense in managing less severe injuries or conditions that do not require immediate surgical intervention.
Medication and Anti-inflammatories: NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) are commonly prescribed to reduce inflammation and pain. Inflammation is a natural response to injury but can cause significant discomfort and impede the healing process. Medications such as ibuprofen and naproxen, by reducing inflammation, contribute to pain relief and are integral in the initial stages of treatment.
Physiotherapy and Physical Modalities: Physiotherapy plays a central role in conservative management, focusing on improving knee mobility, strength, and coordination. Modalities such as ultrasound therapy, electrical stimulation, and ice or heat applications can alleviate pain and enhance tissue healing. Tailored exercise programs aimed at strengthening the quadriceps and hamstrings, crucial for knee stability, are fundamental.
Bracing and Orthotic Devices: In cases of knee instability or specific conditions such as patellofemoral syndrome, bracing or orthotic devices can offer additional support to the knee, redistribute forces away from damaged areas, and allow for safe mobilization.
Activity Modification and Weight Management: For patients experiencing knee issues, especially those derived from or exacerbated by excessive weight or specific activities, advice on activity modification and weight management is vital. Reducing stress on the knee through low-impact activities such as swimming or cycling, combined with a balanced diet to achieve a healthy weight, can significantly decrease symptoms and improve function.
Surgical interventions are considered when conservative treatments are insufficient, or the structural damage is too severe to be managed non-surgically. These procedures aim to repair, reconstruct, or replace areas of the knee that have been damaged.
Arthroscopy: This minimally invasive surgery is utilized for diagnosing and treating a wide range of knee problems. Through small incisions, a camera and surgical tools are inserted, allowing for the repair of damaged tissues, removal of loose bodies, and trimming of torn menisci. The reduced recovery time and minimal scarring are significant advantages.
Ligament Reconstruction: Crucial for knees with ligamentous instability (e.g., ACL tears), these surgeries involve replacing the torn ligament with a graft taken from the patient or a donor. Reconstruction restores stability and functionality, essential for individuals leading active lifestyles or participating in sports.
Osteotomy: In cases of knee osteoarthritis where one side of the knee is more affected, osteotomy surgery can help by reshaping the bones to relieve pressure on the damaged area. This procedure can delay the need for total knee replacement.
Total Knee Arthroplasty (Replacement): Reserved for severe arthritis or damage, knee replacement surgery involves replacing the damaged knee components with artificial parts. This surgery is highly successful in alleviating pain and restoring function in patients with advanced knee problems.
Post-surgery or as part of conservative management, rehabilitation exercises are essential for regaining strength, range of motion, and function in the knee. A tailored rehabilitation program by a physiotherapist can adapt as the patient progresses through their recovery.
Range of Motion Exercises: Starting with gentle range of motion exercises helps in restoring knee mobility without placing undue stress on the healing tissues. Flexion and extension movements, gradually increasing in amplitude, are foundational.
Strengthening Exercises: Quadriceps and hamstrings are pivotal for knee stability. Isometric exercises graduating to resistance training can progressively rebuild muscle strength. Balance and proprioception exercises are also crucial in restoring the knee's dynamic stability and coordination.
Functional Training: Simulating day-to-day activities or sport-specific drills helps in the safe return to pre-injury levels of activity. This phase focuses on ensuring the knee can handle various loads and movements confidently.
Manual Therapy: Techniques such as massage, mobilization, or manipulation by trained therapists can enhance joint mobility, decrease pain, and improve circulation, facilitating a quicker recovery.
In summation, rehabilitation and treatment strategies for the knee must be multifaceted, combining medical, physical, and surgical approaches tailored to the individual's specific condition. Understanding the intricate anatomy of the knee, the nature of the injury or condition, and the patient's lifestyle and goals is crucial in devising an effective treatment plan.
Knee injuries are a frequent concern among individuals engaging in physical activities, whether in sports or in day-to-day life. Given the complex anatomy of the knee, understanding how to prevent these injuries is crucial. The knee's structural components, including its ligaments, tendons, menisci, and bones, work in tandem to provide stability and support while allowing for a range of movements. An injury to any of these parts can lead to pain, limited mobility, and long-term health issues. Thus, this chapter focuses on the prevention of knee injuries through various approaches, encompassing strength and flexibility, protective equipment and techniques, and awareness and education.
Muscular strength and flexibility play pivotal roles in knee joint stability and injury prevention. Strong muscles around the knee, particularly the quadriceps, hamstrings, calves, and hip musculature, provide support and reduce the load on the knee during physical activities. Strengthening these muscles can alleviate the pressure on the knee joint, diminishing the risk of ligamentous injuries and meniscal tears. Exercises such as squats, lunges, and leg presses can enhance muscle strength, while regular stretching enhances flexibility, which is vital for maintaining the range of motion and preventing muscle imbalances.
Flexibility in the muscles and tendons surrounding the knee ensures that movements are smooth and fluid, reducing the risk of strains and tears. Flexibility exercises, including static and dynamic stretching routines before and after physical activities, are beneficial. The elasticity of the muscular and tendinal structures allows for the adequate absorption of forces that are applied to the knee, thereby preventing injuries.
The use of protective equipment can significantly reduce the risk of knee injuries, especially in sports and high-risk activities. Properly fitted and activity-specific knee pads or braces can provide additional support to the knee, absorbing shock and dissipating forces that could otherwise harm the joint and its components. For those with a history of knee injuries, custom-fitted orthotic devices might be prescribed to offer extra protection and support. Additionally, employing correct techniques during sports and physical activities, such as proper landing techniques after a jump or the right way to pivot, can prevent undue stress on the knee.
It is also worth considering the surfaces on which activities are performed. Softer surfaces reduce the impact on the knees compared to hard surfaces. Educating athletes and individuals on the principles of biomechanics involved in their activities can lead to alterations in technique that significantly lower the risk of knee injuries.
Educating individuals about the mechanisms of knee injuries, the importance of warm-up and cool-down exercises, and the significance of gradual conditioning is paramount in injury prevention. Awareness campaigns can provide essential information on understanding the body's limits and recognizing the signs of overuse and fatigue, which are common precursors to knee injuries.
Education on the early signs of knee injuries and the importance of seeking medical advice for persistent knee problems can prevent minor issues from becoming major problems. Moreover, understanding the anatomy and function of the knee enables individuals to appreciate the importance of preventive strategies and adhere to recommended practices for knee health.
Workshops, seminars, and online resources can serve as effective tools for disseminating information on knee injury prevention. These platforms can offer guidance on exercises for strengthening and flexibility, advice on protective equipment, and techniques for safe participation in various activities. Furthermore, they can provide valuable insights into nutritional supports, such as maintaining optimal body weight and ensuring adequate vitamin D and calcium intake for bone health, which indirectly benefits knee joint integrity.
In conclusion, preventing knee injuries requires a multifaceted approach that combines strengthening and flexibility exercises, the use of protective equipment, proper techniques, and comprehensive awareness and education. By understanding the complex structures that comprise the knee joint and employing measures to safeguard these components, individuals can enjoy a range of activities while minimizing the risk of injury. As medical educators, it is our responsibility to impart this knowledge to our students, ensuring they are well-equipped to prevent knee injuries in their future practices.
The text provides an extensive overview of the anatomy, biomechanics, pathologies, treatments, and prevention strategies related to the knee joint, emphasizing its crucial role in human movement and the complexity of its structure. The knee, being the largest joint in the body, is intricately designed to support significant loads while enabling a range of motions crucial for daily activities and athletic endeavors. Detailed descriptions of the knee's components, including bones, cartilages, ligaments, tendons, menisci, and the synovial membrane, underscore the importance of understanding knee anatomy and biomechanics for medical students and professionals to diagnose and manage knee-related conditions effectively.
Pathologies discussed include ligament injuries, meniscal tears, and bursitis, highlighting common causes like trauma, degeneration, or excessive strain. Cruciate and collateral ligaments are particularly emphasized for their role in stabilizing the knee and their susceptibility to sports-related injuries. The text also delves into treatment strategies, contrasting conservative approaches like physiotherapy, bracing, and anti-inflammatory medications with surgical interventions such as arthroscopy, ligament reconstruction, and knee replacement for severe damage or arthritis.
Rehabilitation exercises, crucial for restoring knee function post-injury or surgery, are elaborated, focusing on improving strength, flexibility, and coordination. Additionally, the text advocates for injury prevention through strength building, flexibility exercises, proper use of protective equipment, correct technique during physical activities, and awareness and education on knee health.
In summary, this comprehensive exploration of the knee joint spans its anatomical complexity, the mechanics of its function, common injuries and pathologies, and modern methodologies for treatment and rehabilitation, culminating in practical advice on preventing knee injuries. This serves as an essential resource for medical students, professionals, and anyone interested in understanding knee health and injury prevention.
Anatomy; Biomechanics; Knee; Joint; Flexion; Extension; Rotation; Ligaments; Tendons; Menisci; Bursae; Musculature; Capsule; Synovial Membrane; Patella; Articulation; Genus; Mechanism; Surgery; Rehabilitation; Exercise; Prevention; Injuries; Pathologies; Conservative Treatment; Surgical Interventions. anatomy, biomechanics, knee joint, knee cap, patella, ligaments, tendons, menisci, bursae, musculature, joint capsule, synovial membrane, knee flexion, knee extension, knee rotations, knee inclinations, knee injuries, ligament injuries, meniscal tears, bursitis, rehabilitation, conservative treatments, surgical interventions, preventative measures, strength, flexibility, protective equipment, techniques, awareness, educationUnderstanding Knee Anatomy & Pathologies: A Comprehensive OverviewThe Knee0000