The subclavian artery serves as the principal axial vessel supplying blood to the upper limb. It originates differently on either side of the body: on the right, it arises from the brachiocephalic trunk, and on the left, directly from the aortic arch. The subclavian artery takes various branches catering to structures in the neck and upper chest before transitioning into the axillary artery.
Transitioning at the lateral border of the first rib, the subclavian artery becomes the axillary artery. This name change marks not only a shift in topography but also a shift in clinical relevance – the axillary artery is a key landmark in procedures like lymph node dissection and is prone to injuries associated with shoulder dislocation.
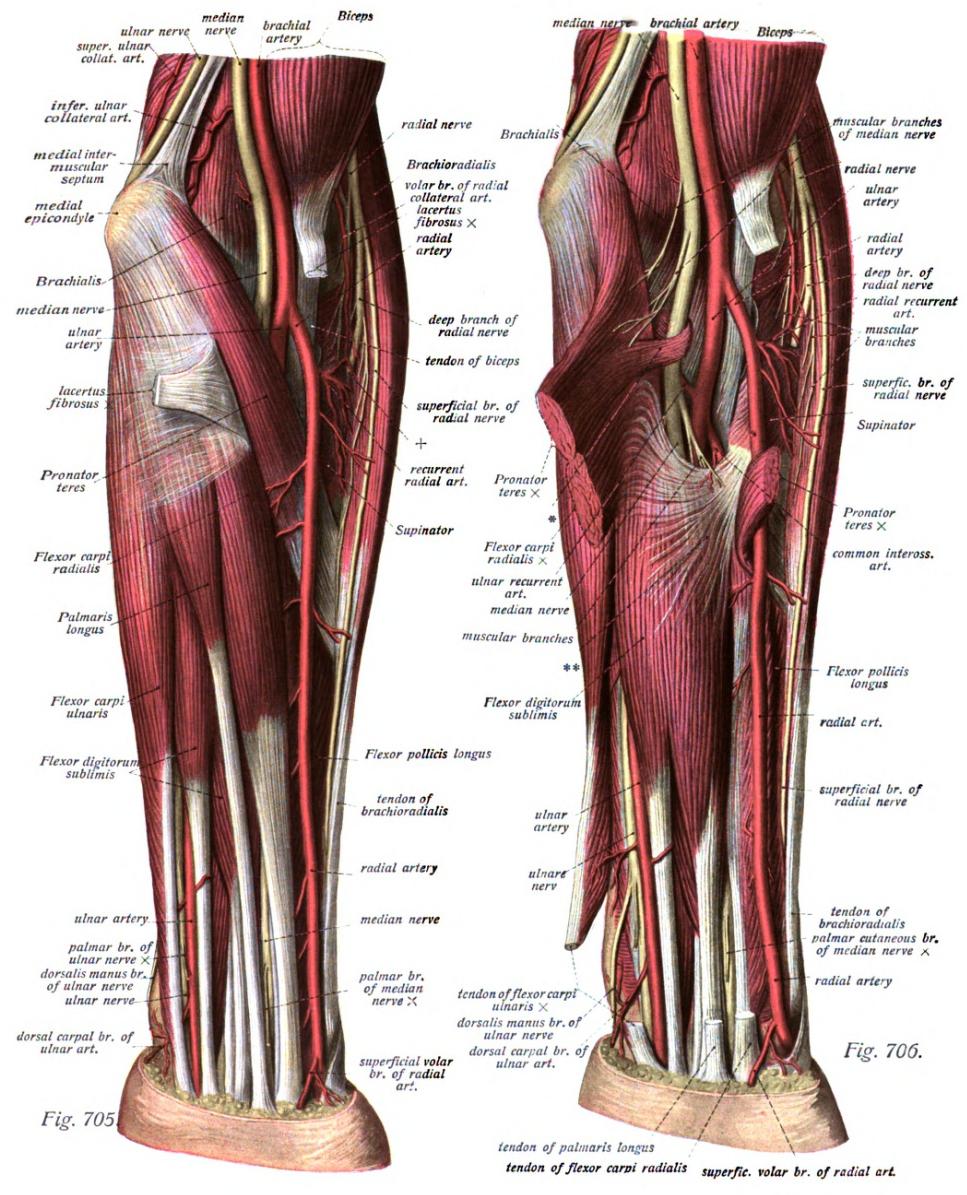
As it passes the inferior margin of the teres major muscle, the axillary artery becomes the brachial artery. The brachial artery supplies the arm and is the vessel most commonly auscultated for blood pressure measurements. It maintains a close anatomical relationship with the median nerve and is accompanied by venae comitantes.
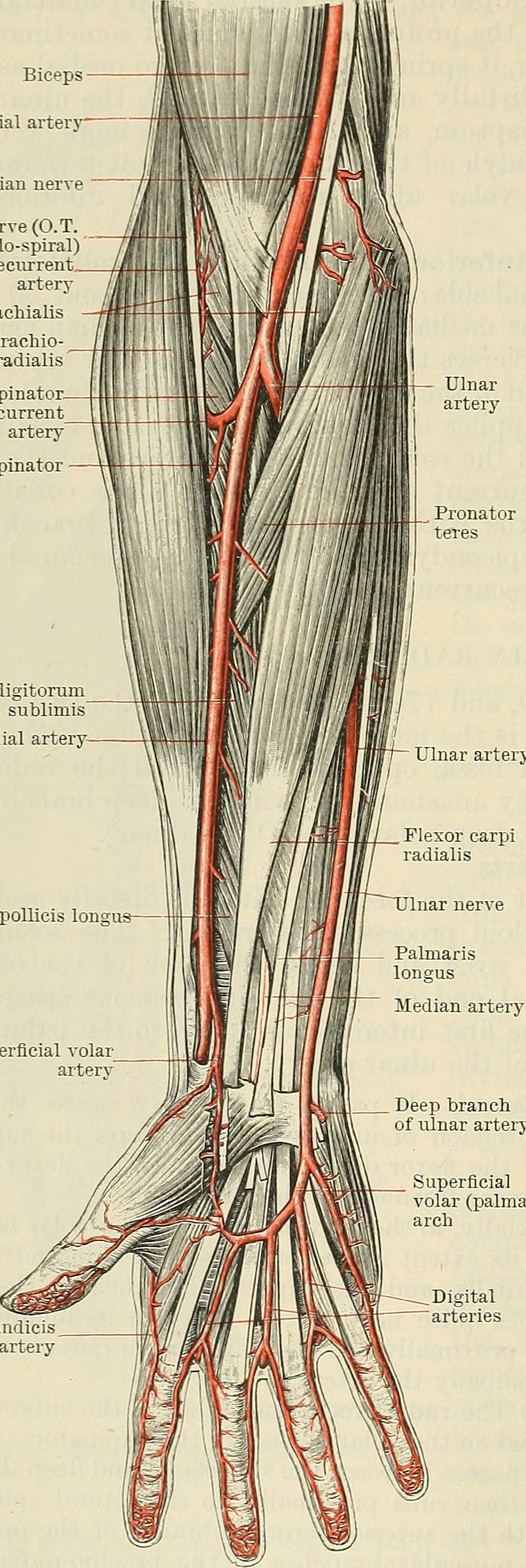
The brachial artery bifurcates into the radial and ulnar arteries just distal to the elbow. The ulnar artery, generally the larger of the pair, continues medially to supply the forearm and hand, with numerous branches anastomosing to maintain blood supply. Conversely, the radial artery travels laterally to contribute to the superficial palmar arch and deep palmar arch, playing a central role in the blood supply to the hand.
Extensive networks of anastomoses exist between the branches of the main arterial vessels, ensuring robust collateral circulation in the upper limb. This collateral system becomes particularly important during instances of arterial occlusion. The interlinking networks enveloping the scapula, elbow, and wrist are essential in maintaining perfusion distally despite proximal arterial occlusions.
Originating from the brachial artery, the profunda brachii artery is specifically tasked with supplying the posterior compartment of the arm, including the triceps muscle, and accompanying the radial nerve through the radial groove. It provides crucial collateral circulation around the elbow via its terminal branches, the radial and middle collateral arteries.
The subclavian artery's pulsation can be palpated at the base of the neck, specifically at the lateral margin of the sternocleidomastoid muscle. This palpation is part of routine physical examinations to check for subclavian artery patency and may offer important clues to thoracic outlet syndrome.
Palpation of the brachial artery is routinely performed in the medial bicipital groove of the arm, between the biceps brachii and the medial head of the triceps brachii. This palpation is not only important for assessing pulse quality and character but also necessary when positioning the cuff for blood pressure measurement.
A thorough examination of the radial and ulnar pulses at the wrist helps to assess the arterial supply to the hand. The radial pulse is typically palpated at the lateral aspect of the wrist, while the ulnar pulse is felt on the medial aspect. The Allen test, which evaluates the patency of the radial and ulnar arteries before procedures like arterial cannulation, is an essential component of this examination.
Understanding the vascular anatomy of the arm is essential for clinical procedures, diagnosis, and management of potential complications. It is a crucial component of medical education, particularly for those entering surgical, emergency, and intrusive diagnostic fields.

The brachial artery is the continuation of the axillary artery below the teres major muscle. This major blood vessel of the upper limb travels down the medial aspect of the arm and is palpable in the medial bicipital groove. Clinically, the brachial artery is where healthcare professionals commonly measure blood pressure using a sphygmomanometer. Its accessibility also makes it a common site for arterial blood gas sampling and catheterization purposes, such as in coronary angiography or cardiac catheterization.
Just distal to the elbow, the brachial artery bifurcates into the radial and ulnar arteries. The ulnar artery is generally larger and primarily contributes to the superficial palmar arch in the hand, whereas the radial artery, smaller and running along the lateral aspect of the forearm, contributes to both the deep and superficial palmar arches. These vessels provide the hand's peripheral blood supply, enabling a rich, redundant system that sustains limb function.
The radial and ulnar arteries are the primary arteries responsible for supplying blood to the hand. The radial artery travels dorsally between the carpal ligaments and the tendons of the thumb extensors, while the ulnar artery follows a course deep to the flexor retinaculum and lateral to the ulnar nerve and pisiform.
Arterial cannulation at the radial artery is a common practice for continuous blood pressure monitoring and repeated arterial blood sampling, due to its superficial course and ease of access. Additionally, non-invasive blood pressure measurements typically involve the compression of the brachial artery against the humerus, whereby the cessation and return of blood flow are correlated with systolic and diastolic pressure readings, respectively.
In the arm, the median nerve travels medially to the brachial artery. This close proximity has implications for clinical practices: inadvertent injury to the median nerve during brachial artery puncture can occur if not carefully avoided. Hence, it is critical to understand the anatomic relationship between these two structures when performing any invasive procedure in this region.
The compact anatomy of neurovascular structures within the arm not only includes potential injury during procedures such as arterial puncture or venipuncture but also encompasses clinical conditions. For instance, compartment syndrome, which can result from trauma, can compromise circulation and necessitate emergency intervention to prevent permanent damage. Intracompartmental pressures must be monitored, with fasciotomies performed when indicated. Another consideration is the susceptibility of the radial artery to vasospasm or thrombosis, though collateral circulation typically preserves hand perfusion. Awareness of these conditions and the anatomy informing them is vital for clinical acumen and patient care.
The skin of the upper limb receives its blood supply through three main pathways: direct cutaneous vessels, musculocutaneous perforators, and fasciocutaneous vessels. These pathways ensure a rich blood supply critical for tissue health, especially valuable in skin grafts and flaps.
The fasciocutaneous system derives its flow from the source arteries and passes along intermuscular septa, serving extensive areas of skin. This network's robustness provides the anatomical basis for the design of various fasciocutaneous flaps. These flaps are crucial for covering defects that have resulted from trauma or resection, supporting not just the survival of the transferred tissue but also enhancing nerve regeneration and ameliorating neuropathic pain due to rich vascularity.
The direct cutaneous arteries, such as those that supply the palmar skin from the underlying digital vessels, offer a more straightforward flow to the skin. The palmar aspect of the hand benefits from such consistent and uncomplicated supply, making it an area less susceptible to ischemic complications and a reliable site for flap harvest.
Medical students must grasp the complexity of vascular anatomy when considering interventions that involve skin flaps for reconstructive surgery. The upper limb's blood supply not only assures tissue viability but also enables intricate reconstructive techniques, vital for restoring form and function after trauma or surgical interventions.
Understanding the vascular supply is pivotal in plastic and reconstructive surgery, particularly for the latissimus dorsi myocutaneous flap, which hinges on the thoracodorsal vessels. The deep and direct supply allows for various reconstructive techniques involving cutaneous or musculocutaneous flaps. These are used to cover large defects, re-establish form and function, and even provide musculofascial support thanks to the interconnected vascular territories that facilitate intricate anastomoses.
In reconstructive surgery, the latissimus dorsi myocutaneous flap, based on the thoracodorsal vessels, holds a place of significance. Harvested with an overlaying skin paddle, it provides substantial soft tissue for coverage of defects in the upper limb and other regions. This vascularized flap leverages the underlying muscle's consistent vascular supply to support tissue healing and is especially useful in complex reconstructions necessitating robust and well-vascularized coverage.
The intricate network of anastomoses and the potential for arterial variation in the hand and wrist are crucial to the comprehensive understanding of vascular supply. This complexity not only empowers the upper extremity's robustness to injury but also complicates surgical and emergency interventions.
The arterial system of the hand is characterized by a remarkable network of anastomoses, particularly between the radial and ulnar arteries, which is pivotal for maintaining blood flow despite vessel occlusion. These anastomoses form two fundamental arches: the superficial palmar arch, primarily contributed to by the ulnar artery, and the deep palmar arch, predominantly formed by the radial artery. These palmar arches connect via their digital branches, ensuring rich and redundant perfusion to the hand, which is essential for tissue viability and healing.
The radial artery travels along the lateral aspect of the forearm, traversing from the deep radial groove outwards to the anatomical snuffbox, then onward to participate in both superficial and deep palmar arches after giving off several branches. One particular branch of note is the radial recurrent artery, which establishes proximal collateral flow. Knowledge of the radial artery’s course is critical when performing procedures such as arterial cannulation or managing traumatic injuries.
The palmar carpal arch forms through the anastomosis between the palmar carpal branch of the radial artery and the ulnar artery. Similarly, the dorsal carpal arch is created from anastomotic branches including the dorsal carpal branch of the radial artery. These arches provide blood supply to the carpal bones and the intracarpal articulations and give rise to dorsal metacarpal arteries, which in turn contribute to the vascular supply of the dorsal hand.
The palmar metacarpal arteries run distally from the convexity of the deep palmar arch across the interossei of the second to fourth spaces, contributing to the arterial supply of the fingers. These arteries join the common digital branches of the superficial arch at the digital clefts, forming an intricate network that ensures proper blood perfusion to the digits. Additionally, the palmar metacarpal arteries display anastomoses with the dorsal metacarpal arteries and contribute to the overall vascular supply of the hand. This complex network of arteries ensures that the thumb and fingers receive the necessary oxygen and nutrients for optimal functioning.
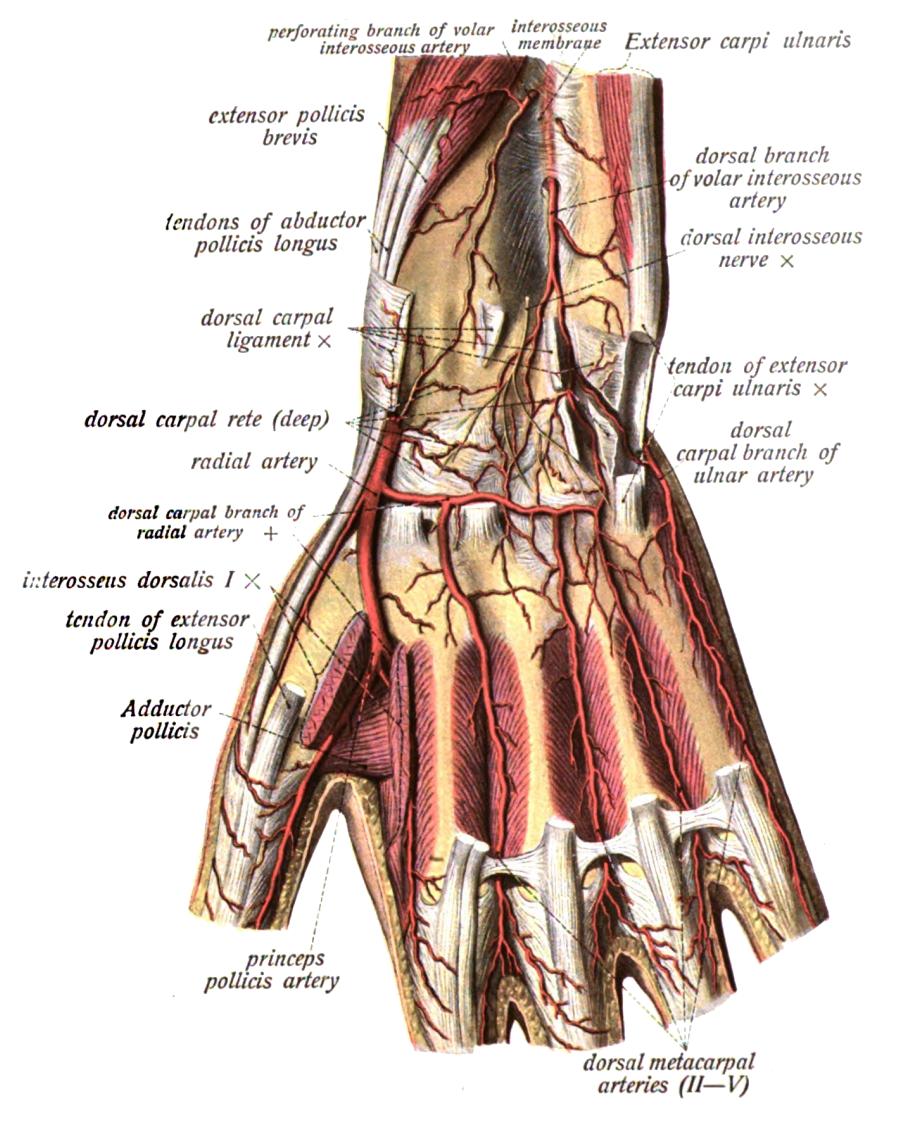
The deep palmar arch is formed by the anastomosis of the end of the radial artery with the deep palmar branch of the ulnar artery. This arch crosses the bases of the metacarpal bones and interossei, providing a robust blood supply to the deep structures of the hand. Covered by the oblique head of adductor pollicis, the tendons of the digital flexors, and the lumbricals, the deep palmar arch ensures that the muscles and other vital structures in the hand receive adequate oxygen and nutrients to function optimally.
Dorsal metacarpal arteries originate from the dorsal carpal arch and divide into dorsal digital branches, supplying the sides of the fingers. The first dorsal metacarpal artery, in particular, is notable as it provides blood to the radial side of the thumb and index finger, paralleling the course of the bone and demonstrating potential intramuscular routing. These dorsal metacarpal arteries anastomose with their palmar counterparts, ensuring a generous blood supply to the digits, which is essential for the survival of local tissues and any reconstructive grafts or flaps.
The intrinsic muscles of the hand receive their vascular supply from specific branches of the radial and ulnar arteries. The flexor pollicis brevis, abductor pollicis brevis, opponens pollicis, and adductor pollicis are supplied by branches including the superficial palmar branch of the radial artery, arteria princeps pollicis, and arteria radialis indicis. The abductor digiti minimi, flexor digiti minimi brevis, and opponens digiti minimi are primarily supplied by the deep palmar branch of the ulnar artery, along with branches from the superficial palmar arch's ulnar end. These specific vascular pathways ensure adequate blood supply to the intricate and delicate muscles of the hand, allowing for proper function and movement.
The blood supply to the intrinsic hand muscles is tailored to the unique needs of each muscle group. For example, the abductor pollicis brevis and flexor pollicis brevis receive branches from the superficial palmar branch of the radial artery, ensuring sufficient oxygen and nutrients reach these critical muscles involved in thumb movement. Similarly, the abductor digiti minimi and opponens digiti minimi rely on the deep palmar branch of the ulnar artery to supply them with the necessary blood flow. Understanding these specific vascular supply patterns is essential for medical students to grasp the intricate anatomy and physiology of the hand muscles.
Anastomoses between the radial and ulnar arteries form a vital network of connections in the hand and wrist, ensuring continuous blood supply to these crucial areas. These connections, such as the palmar and dorsal carpal arches formed by anastomoses between the radial and ulnar arteries, play a significant role in maintaining blood flow to the hand and fingers. Understanding the location and significance of these anastomoses is essential for medical students to comprehend the complex vascular network that supports the hand's functionality and health.
The arterial supply to the thumb is primarily provided by the arteria princeps pollicis, which arises from the radial artery as it enters the palm, forming the deep palmar arch. This artery descends along the palmar surface of the first metacarpal, supplying the thumb with blood. Additionally, the first dorsal metacarpal artery, a derivative of the radial artery, contributes to the arterial supply of the thumb. It runs over the first dorsal interosseous muscle and parallel to the second metacarpal bone, occasionally taking an intramuscular path. The radial side of the thumb also receives a direct branch from the radial artery, ensuring adequate blood flow to this important digit.
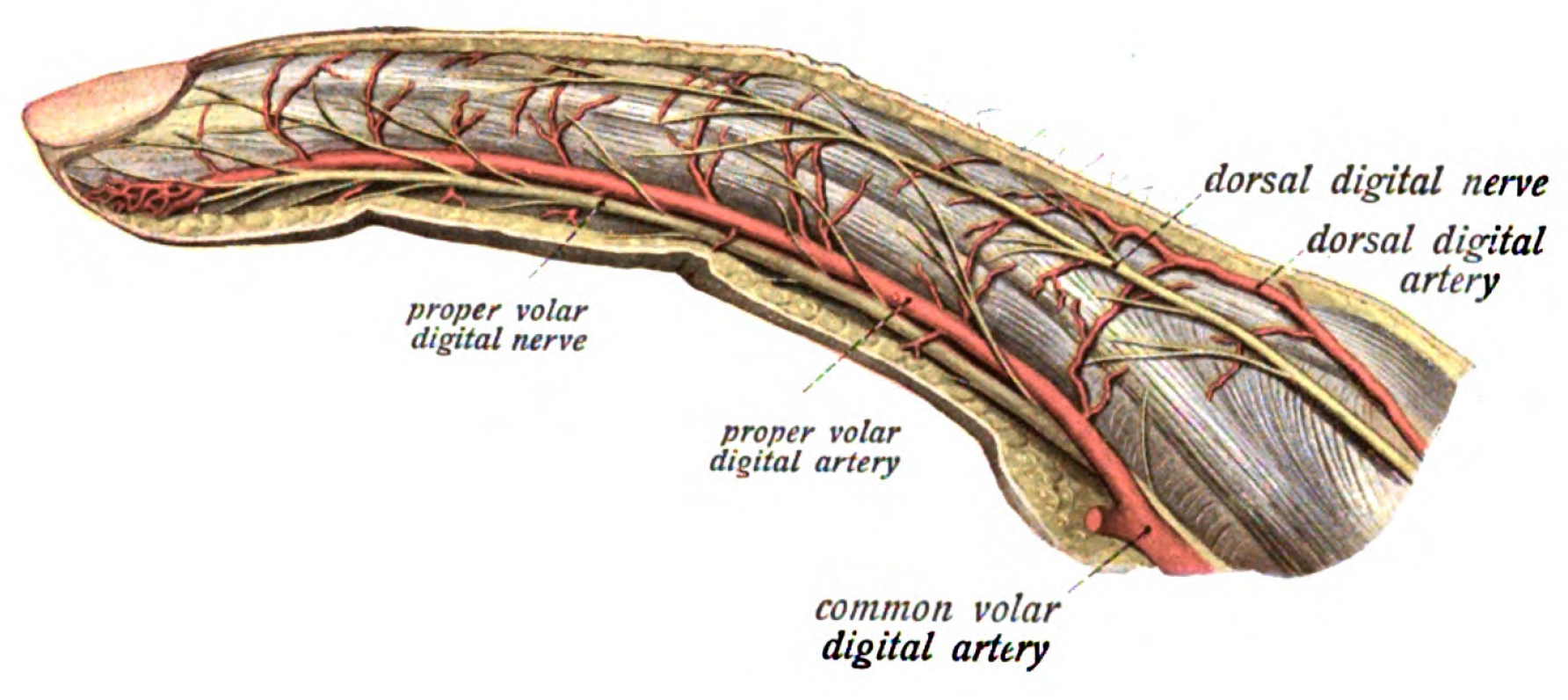
The arteria radialis indicis plays a crucial role in the arterial supply to the index finger. This artery can arise from various sources, including the arteria princeps pollicis, the superficial arch, or the first dorsal metacarpal artery. As it descends between the first dorsal interosseous muscle and the transverse head of the adductor pollicis muscle, the arteria radialis indicis provides blood to the lateral side of the index finger, ensuring optimal perfusion to this digit. It anastomoses with the index medial digital artery, arteria princeps pollicis, and the superficial palmar arch, contributing to the intricate vascular network in the hand.
The vascular system of the upper limb includes superficial and deep venous networks that facilitate blood return to the heart. The superficial veins are prominent under the skin and often utilized for medical procedures like venipuncture. In contrast, deep veins accompany main arteries and carry the bulk of the venous return, shielded by muscle and fascial layers. A sophisticated array of valves in these veins ensures unidirectional blood flow, countering the effects of gravity during limb elevation. Due to their proximity to the arterial supply, deep veins significantly contribute to thermoregulation by heat exchange between arterial and venous blood.
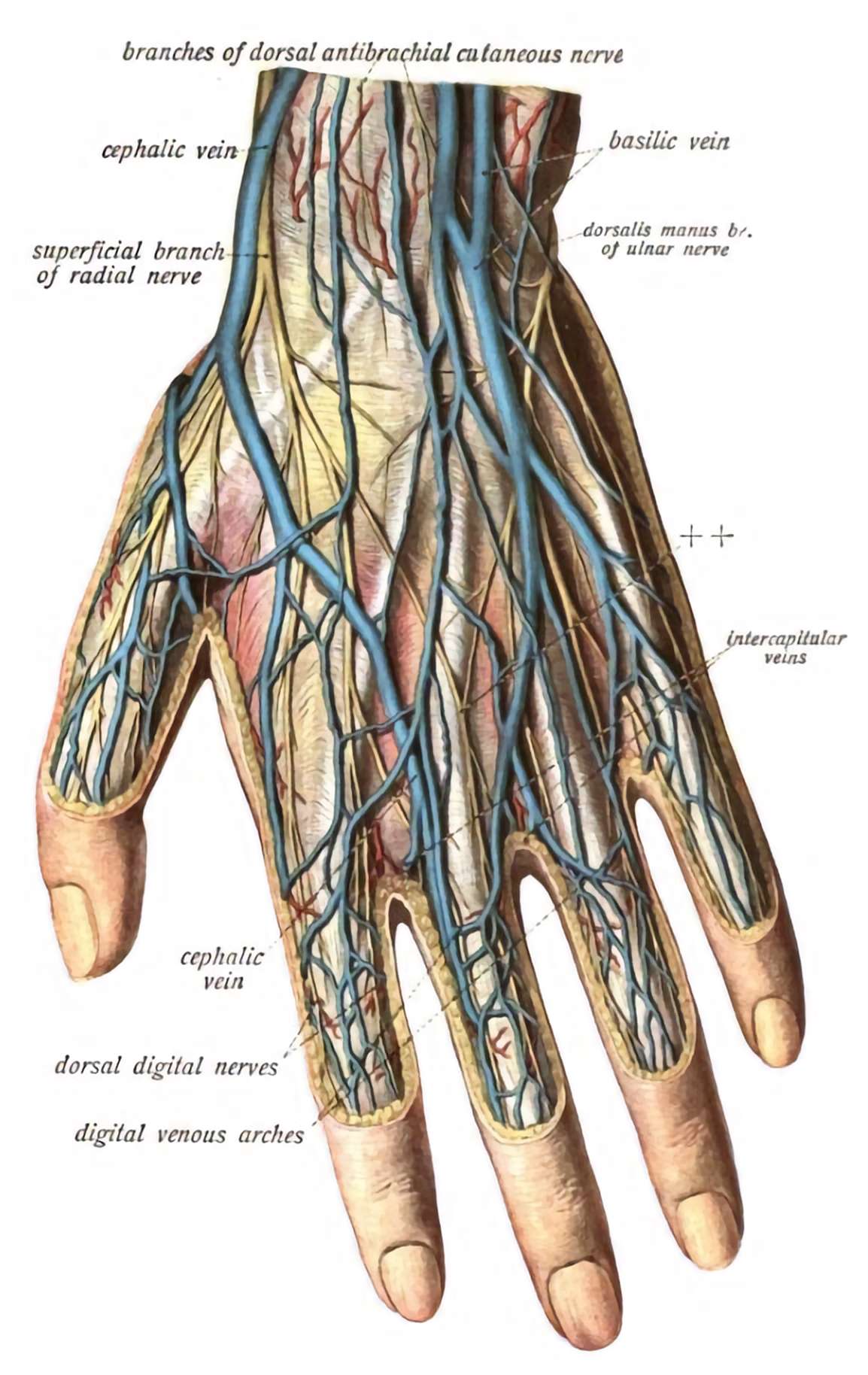
Originating on the dorsal surface of the hand is the dorsal venous arch, a critical superficial structure in the drainage system of the upper limb. This arch collects blood from the digital veins and channels it into larger veins of the forearm. It serves as a junction where the cephalic vein begins laterally and the basilic vein starts medially, each following the contours of the upper limb and emptying into the deep venous system proximally. The visibility of the dorsal venous arch, cephalic, and basilic veins make them accessible for procedures such as cannulation and venipuncture.
The cephalic vein, conspicuous along the radial border of the forearm, ascends from the dorsal venous arch and courses along the lateral aspect of the biceps brachii to eventually drain into the axillary vein. This vein is commonly used for intravenous access because of its superficial location and relatively consistent anatomy. It travels through the deltopectoral triangle, making it palpable in the infraclavicular fossa, important during central venous catheterization procedures.
The basilic vein arises from the ulnar side of the dorsal venous arch and courses medially in the forearm and arm, later joining deep veins to become part of the axillary vein. The median cubital vein, frequently selected for blood sample collections due to its superficial position, bridges the cephalic and basilic veins across the cubital fossa. This region's rich venous anastomoses provide collateral circulation pathways vital for maintaining upper limb blood drainage even when some venous segments are compromised.
Deep venous drainage involves the deep median vein, which emerges from the palmar venous plexuses and typically joins with the venae comitantes of the brachial artery. Ultimately, they coalesce to form the subclavian vein beneath the clavicle, a nexus point where upper limb venous blood returns to the central circulation system. The subclavian vein also receives contributions from the external jugular and thoracic veins, aiding in efficient blood return from the upper limb.
The risk of air embolism is a critical concern during procedures involving the subclavian, external, or internal jugular veins. An air embolism can occur if venous pressure at the puncture site is less than atmospheric pressure, inadvertently introducing air into the circulation. This potential complication requires careful technique, including Trendelenburg positioning and air-tight sealing of catheters during central line insertions, to prevent air entrainment into the venous system.
The thoracic duct and right lymphatic duct represent the main lymphatic vessels of the body, draining lymph from the upper limbs into the venous system near the subclavian vein and internal jugular vein junction. The thoracic duct primarily drains the left side of the body and the upper left limb, while the right lymphatic duct functions similarly for the right side. These vessels ensure immune surveillance and fluid balance, filtering lymph before reintroducing it into the bloodstream.
This lesson provides a comprehensive summary of the vascular anatomy, pathology, clinical considerations, and surgical implications of the upper limb, spanning from arteries and veins to lymphatic drainage.
The arterial supply starts with the subclavian artery, which becomes the axillary and then brachial artery as it moves down the limb. Key branches, including the radial and ulnar arteries, supply the arm and hand, forming vital anastomoses like the superficial and deep palmar arches. Palpable pulse points along these vessels are essential for clinical assessments and procedures.
The venous system features superficial and deep veins, including the cephalic and basilic veins, important for venous return and as access points for venipuncture. The subclavian vein serves as a major drainage pathway, merging with the internal jugular vein to form the brachiocephalic vein. The lymphatics parallel the venous system, draining lymph fluid and supporting immune function.
Pathologies like compartment syndrome and glomus tumors present unique clinical challenges. Compartment syndrome involves increased pressure within muscle compartments, leading to ischemia and can necessitate a fasciotomy. Glomus tumors, painful nodules typically found in the fingers, are treated surgically.
Reconstructive implications address skin vascularization, myocutaneous and fasciocutaneous flaps, critical for repairing defects. Myocutaneous flaps maintain blood supply to both muscle and overlying skin, while fasciocutaneous flaps utilize an extensive anastomotic network for wound treatment.
Finally, clinical correlations discuss arterial catheterization practices, compartment syndrome, the importance of understanding brachial plexus-vascular proximity during surgeries, and the significance of recognizing arterial branching variations to avoid surgical complications and improve outcomes.
Subclavian Artery, Brachial Artery, Axillary Artery, Teres Major, Ulnar Artery, Radial Artery, Palpable Pulse Points, Blood Supply, Collateral Circulation, Profunda Brachii, Thoracoacromial Artery, Subscapular Artery, Posterior Compartment, Anastomoses, Interconnections, Radial-Ulnar Arteries, Wrist, Hand, Superficial Veins, Deep Veins, Superficial Palmar Arch, Deep Palmar Arch, Median Cubital Vein, Lymphatic Drainage, Compartment Syndrome, Skin Vascularization, Myocutaneous Flaps, Fasciocutaneous Flaps, Arterial Catheterization, Ischemic Pain, Brachial Plexus, Vascular Anomalies, Arterial BranchingThe Upper Limb Vascular Anatomy and Clinical ConsiderationsBlood supply of the upper limb0000