The placenta is a feto-maternal organ that consists of two components: a large fetal portion and a small maternal portion. It functions as a transport mechanism between the mother and the fetus. The placenta and umbilical cord perform several functions including protection, nutrition, respiration, excretion, and hormone production. At birth, the placenta and fetal membranes are expelled from the uterus.
During pregnancy, the placenta serves as an organ that allows the fetus to receive nutrients and eliminate waste. It is a pregnancy-created organ with a spongy vascular structure, dark red in color, and filled with blood. The placenta connects the mother and fetus, ensuring necessary physiological exchanges for nutrition and development.
Placental formation begins in the early weeks of pregnancy and reaches functional maturity by the end of the third month. The placenta is formed by the union of an ovular element, known as the fetal placenta, and a maternal element, known as the maternal placenta.
The mature placenta consists of fetal villi that develop in an intervillous space filled with maternal blood. The fetal blood in the villous vessels exchanges substances with maternal blood along the villous wall. These substances are primarily nutritional, but the placenta also secretes hormones, including sex steroids that maintain pregnancy. Maternal antibodies cross the placenta to protect the fetus against infections. The placenta grows along with the fetus and at birth, it weighs approximately one-sixth of the fetal weight.
Formation of the Decidua: As the blastocyst implants into the uterine wall, the endometrial stroma forms the decidua.
Placental development begins when the implanted blastocyst induces decidual reaction in the maternal endometrium, causing the endometrium to become a compact, nutritious, and highly vascularized tissue called the decidua. From the second month, the growing embryo begins to protrude into the uterine lumen. This prominent face of the embryo is covered by a thin capsule of decidua called the capsular decidua, which later disintegrates. When the fetus fills the uterine cavity and starts protruding into the uterine lumen in the second month, the villi on the prominent, non-embryonic side of the chorion disappear; this region of the chorion is now called the smooth chorion or chorion laeve, while the chorion portion associated with the basal decidua retains its villi and is called the frondosum chorion (from Latin "frondosum" meaning fluffy).
The placental villi continue to grow during the majority of the remaining gestation period. Starting from the ninth week, tertiary stem villi elongate through the formation of terminal mesenchymal villi, which originate as syncytiotrophoblast buds (trophoblastic buds) similar in cross-section to primary stem villi. These terminal extensions of the tertiary stem villi reach their maximum length at week 16 and are called intermediate mature villi. The cells of the cytotrophoblastic layer become more dispersed in these villi, leaving openings in the wall of the villous tree. At the end of the second trimester, tertiary stem villi also form numerous thin branches called mature intermediate villi. The first formed mature intermediate villi complete their formation in week 32 and begin to form small secondary branches, resembling nodules, called terminal villi. These complete the structure of the placental villous tree. It is suggested that terminal villi do not form through active growth of the syncytiotrophoblast, but rather through the coalescence and curling of the villous capillaries protruding on the villous wall.
The placenta is made up of various components and structures that play important roles in fetal development and maternal blood circulation. The intervillous space, which contains blood and villi, is created by trophoblastic lacunae that grow and merge together. This space is lined on both sides by syncytiotrophoblast. On the maternal side of the placenta, there is a trophoblast margin and a supportive layer of basal decidua, known as the basal plate. On the fetal side, the chorion forms the chorionic plate.
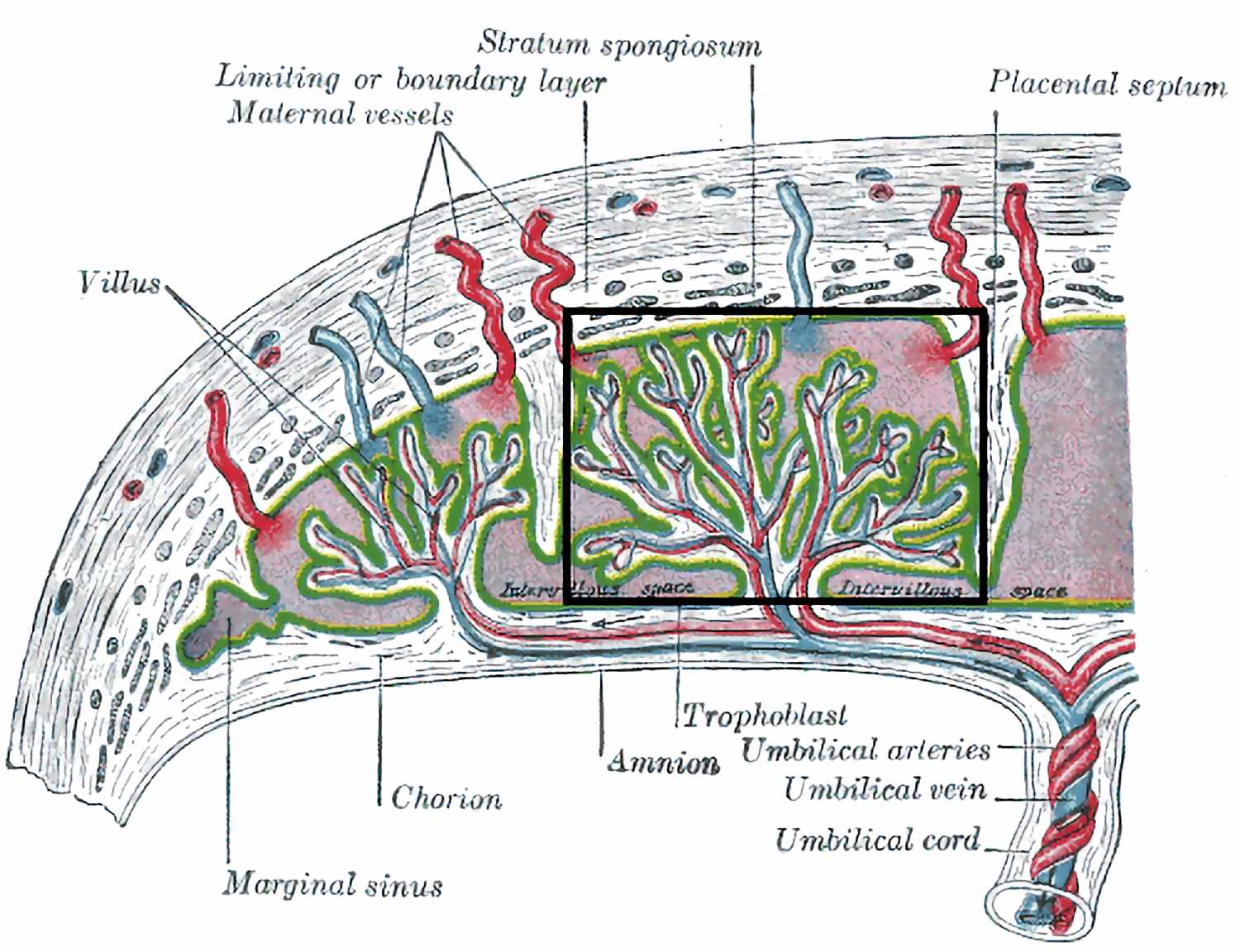
Placental septa, made of decidual tissue, divide the placenta into cotyledons. These septa grow into the intervillous space, separating the villi into groups called cotyledons. Importantly, the placental septa do not merge with the chorionic plate, allowing maternal blood to freely circulate between cotyledons.
As the fetus grows, the uterus and placenta expand. The placenta thickens until around 18 weeks of gestation, covering 15-30% of the decidua. The fetal component of the placenta consists of chorionic villi, with stem villi protruding into the intervillous space filled with maternal blood. The maternal component is composed of basal decidua, which is the endometrium in contact with the fetal component. By the end of the fourth month, the basal decidua is mostly replaced by the fetal component of the placenta.
The fetomaternal junction involves the attachment of the fetal portion of the placenta (villous chorion) to the maternal portion. This attachment is facilitated by cytotrophoblastic envelopes. The chorionic stem villi are firmly anchored to the basal decidua by these envelopes, securing the chorionic sac and placenta. Maternal arteries and veins pass through openings in the cytotrophoblastic envelope, allowing them to open into the intervillous space.
The placenta's appearance is determined by the shape of the persistent area of the chorionic villi. Typically, this area is circular, giving the placenta a discoid appearance. As placental formation occurs and the chorionic villi invade the basal decidua, the endometrial tissue is eroded to enlarge the intervillous space. This process creates placental septa, which are prominent areas of decidual tissue that protrude onto the chorionic plate. These placental septa divide the fetal part of the placenta into irregular, convex areas called cotyledons. Each cotyledon visible on the maternal surface of the placenta consists of two or more stem villi and branches. By the fourth month, the basal decidua is almost completely replaced by cotyledons.
The decidua capsularis, which is the superficial part of the decidua facing the conceptus, forms a capsule above the external surface. As the conceptus grows, the decidua capsularis protrudes into the uterine cavity, eventually making contact and fusing with the decidua parietalis, which obliterates the uterine cavity. At 22 weeks, reduced blood supply to the decidua capsularis leads to its degeneration and disappearance.
The intervillous space, which is filled with maternal blood, is derived from lacunae that develop in the syncytiotrophoblast during the second week. These lacunae enlarge and coalesce, forming compartments that are divided by the placental septa. However, these compartments freely communicate with each other because the septa do not reach the chorionic plate.
Maternal blood enters the intervillous space through the spiral arteries in the basal decidua. These endometrial arteries pass through openings in the cytotrophoblastic shell and discharge blood into the intervillous space. From there, the blood is drained into the endometrial veins that also penetrate the cytotrophoblastic shell. The villous branches are continuously bathed in maternal blood circulating through the intervillous space, allowing for gas and nutrient exchanges to take place.
The amniochorionic membrane is formed as the amniotic sac grows faster than the chorionic sac. This results in the fusion of the amnion and chorion, forming the amniochorionic membrane, which then fuses with the decidua capsularis. After the degeneration of the decidua capsularis, the amniochorionic membrane fuses with the decidua parietalis. During labor, the amniochorionic membrane ruptures. Premature rupture of this membrane, also known as water breaking, often leads to premature labor. When the amniochorionic membrane ruptures, amniotic fluid exits through the cervix and vagina.
The fetal placental circulation involves the movement of poorly oxygenated blood from the fetus to the placenta through the umbilical arteries. These arteries divide into radiating vessels that branch in the chorionic plate before entering the villi. This creates an extensive arterio-capillary-venous system that brings fetal blood close to maternal blood, allowing for exchange between the two. Normally, there is no mixing of maternal and fetal blood, but there can be small amounts of fetal blood entering the maternal circulation due to defects in the placental membrane. Well-oxygenated fetal blood then passes into thin-walled veins that follow the placental arteries and converge to form the umbilical vein, which carries oxygen-rich blood and nutrients to the fetus.
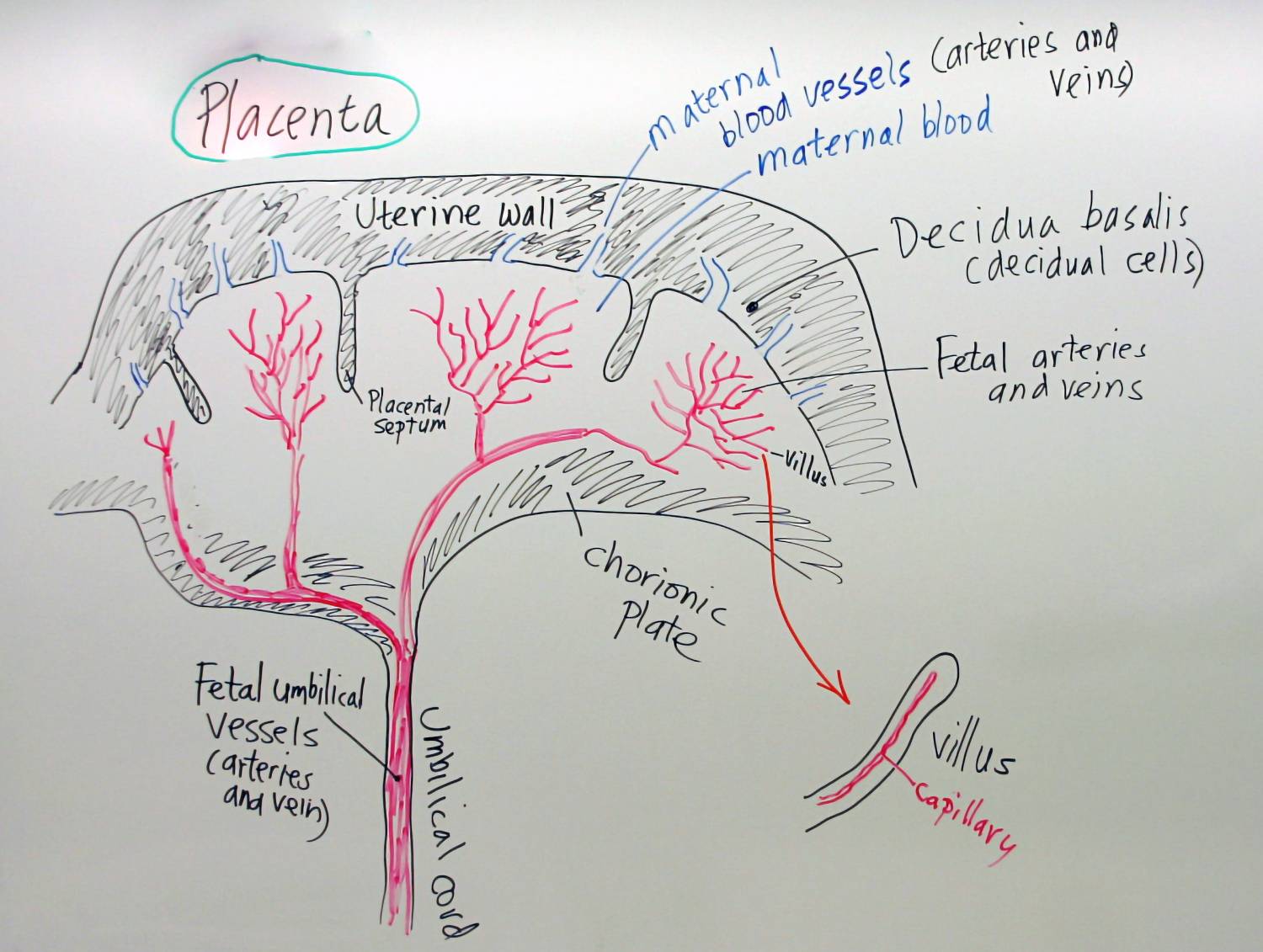
On the other hand, the maternal placental circulation involves blood from the intervillous space, which is temporarily located outside the maternal circulatory system. This blood enters the intervillous space through spiral arteries from the decidua basalis, passing through the cytotrophoblastic layer. The blood in the spiral arteries is pulsatile and propelled in jets by the pressure of maternal blood. It enters the intervillous space with higher pressure than that within the space, rushing towards the chorionic plate and forming a sort of ceiling. As the pressure decreases, the blood flows slowly around the villous branches, allowing for the exchange of gases and metabolites with fetal blood. It then returns to the endometrial veins and the maternal circulation.
The adequate supply of blood from the maternal circulation to the villous branches is crucial for the normal growth of the fetus. Reduction in utero-placental circulation, caused by factors such as nicotine, can result in fetal hypoxia and slowed growth, and severe reduction can even lead to fetal death. The intervillous space of the maternal placenta contains approximately 150 ml of blood, which is replaced 3-4 times per minute. Uterine contractions during pregnancy decrease utero-placental blood flow, but do not significantly increase blood in the intervillous space. This means that the transfer of oxygen to the fetus is reduced during uterine contractions, but not completely halted.
The placental membrane is composed of four layers: syncytiotrophoblast, cytotrophoblast, connective tissue from chorionic villi, and endothelium of fetal capillaries. However, after week 20, histological changes occur, resulting in the thinning or disappearance of the cytotrophoblastic layer. This leaves only large areas of syncytiotrophoblast, reducing the placental membrane to three layers in most areas.
Although commonly referred to as a placental barrier, this term is inaccurate as only a few substances are unable to cross it. The placental membrane acts as a true barrier only for molecules with specific size, configuration, and charge, such as heparin, certain metabolites, toxins, and hormones.
Most drugs and substances in maternal plasma can cross the placental membrane and enter fetal blood. As pregnancy progresses, the membrane becomes thinner and more permeable. In some areas, syncytiotrophoblast nuclei gather in nuclear aggregates that break down and are transported into maternal circulation. These aggregates are then destroyed by local enzymes in the maternal lung.
Towards the end of pregnancy, a fibrinoid material composed of fibrin and other intensely stained materials forms on the surface of the villi. This material appears to have a negative impact on placental functions.
After birth, the placenta typically has a discoidal shape, measuring 15-20 cm in diameter and 2-3 cm in thickness. It weighs around 500-600 grams, which is roughly 1/6 of the fetus's weight. The edges of the placenta are connected to the ruptured amniotic sac and chorionic sacs.
During the development of the placenta, the chorionic villi only persist in areas where the villous chorion is in contact with the decidua basalis. If the villi persist in other areas, various changes can occur in the placenta, such as accessory placentas, bidiscoidal placentas, diffuse placentas, and ladder-shaped placentas. While there are different variations in the shape of the placenta, most of them have little physiological or clinical significance.
However, examining the placenta after birth can provide valuable information regarding placental dysfunction, fetal growth restriction, congenital diseases, and infant death. It helps determine if the placenta is complete or if there is retention of cotyledons or an accessory placenta, which can lead to uterine hemorrhage.
Choriocarcinoma is a condition where abnormal proliferations of the syncytiotrophoblast occur in some cases of cytotrophoblast, leading to the formation of malignant tumors. These tumors invade the basal decidua, penetrate blood vessels and lymphatics, and metastasize to various organs including the lungs, bone marrow, and liver. Fortunately, gestational choriocarcinomas are highly responsive to chemotherapy and can be cured.
The maternal surface of the placenta is characterized by cotyledons, which are separated by grooves that used to be occupied by placental septa. The cotyledons are covered by thin portions of basal decidua. While most of the decidua is temporarily retained in the uterus, it will be eliminated during the subsequent bleeding.
The placenta is a vital organ in pregnancy that allows for the exchange of gases, nutrients, metabolic products, and antibodies between the mother and fetus. On the fetal surface of the placenta, the umbilical cord is attached and is connected to the amnion, which is also attached to the chorionic plate. The chorionic vessels can be seen through the transparent amnion, radiating towards and from the umbilical cord. These vessels branch out on the fetal surface to form the chorionic vessels that enter the villi.
Approximately 100 spiral arteries allow maternal blood to enter the intervillous spaces of the placenta, while the endometrial veins return the blood back. The placenta contains around 150 ml of maternal blood, which is replaced 3-4 times per minute. Within the placenta, nutrients and oxygen pass from the maternal blood through the layers of the villous wall into the fetal blood. On the other hand, metabolic waste products such as carbon dioxide, urea, uric acid, and bilirubin flow from fetal blood to maternal blood.
One important function of the placenta is the transfer of antibodies from the mother to the fetus. These antibodies pass through the placenta and enter the fetal circulation, providing passive immunity against certain infections like diphtheria and measles. These transferred antibodies remain in the child's blood for several months after birth, offering protection until the child's own immune system develops fully.
The placenta, while generally impermeable to microorganisms, can still allow the passage of certain viral and bacterial pathogens. This means that several bacteria and viruses have the ability to cross the placenta and infect the fetus. Since the fetus lacks a functional immune system, it relies on maternal antibodies for protection and is largely defenseless against infections. Consequently, even a mild infection in the mother can have severe consequences for the fetus, including death.
Among the viruses that can cross the placenta are rubella virus (causing rubella), varicella-zoster virus (causing chickenpox), cytomegalovirus (causing mononucleosis), and Coxsackie virus (causing various mild diseases in adults). If these viruses infect the embryo during early development, they can lead to abortion. Infections that occur later in pregnancy can result in a range of abnormalities, such as blindness, microcephaly, and mental retardation.
Another bacterium that can cause congenital infections is Treponema pallidum, the agent of syphilis, which easily crosses the placenta. Additionally, human immunodeficiency virus (HIV) can be transmitted to the fetus during childbirth or through breast milk, leading to acquired immune deficiency syndrome (AIDS) and associated syndromes. HIV can infect the fetus by crossing the placenta or through breast milk during lactation. Infants born with HIV may appear healthy initially but typically succumb to the disease around the age of 3. Similar to adults, HIV destroys the immune system in children, making them susceptible to recurring infections such as parotid gland infections, diarrhea, bronchitis, and middle ear infections. Pneumocystis carinii pneumonia, which is a characteristic infection in adults with AIDS, is particularly alarming in children, as it often leads to death within 1-3 months.
According to the American Centers for Disease Control and Prevention (CDC), in 2019, over one million people were infected with HIV, and 1% of these infections were acquired during pregnancy or childbirth. [4]
Teratogenic agents, which can cause specific congenital anomalies or hinder fetal growth, play a significant role in prenatal development. These agents are able to reach the fetus by crossing the placenta.
Identifying teratogenic substances is a challenging task due to their complex nature. To determine their effects, researchers rely on epidemiological studies and experiments involving pregnant animals. However, difficulties arise because most congenital malformations have a multifactorial etiology. The development of such malformations depends on both exposure to teratogenic agents and the genetic characteristics of individuals. Interestingly, the same dose of a teratogen can cause severe abnormalities in one person while having no effect on another. Additionally, malformations primarily occur during the "sensitive period" when the embryo undergoes morphogenesis. This vulnerable period, which is characterized by significant organogenesis events, takes place during the first weeks of development.
Teratogenic therapeutic drugs include retinoids (such as vitamin A and analogues), warfarin anticoagulants, trimethadione and phenytoin anticonvulsants, as well as various chemical agents used in cancer treatment. These drugs primarily exert their effects during the embryonic period. However, it is worth noting that many anesthetics and other medications can also impact the health of the fetus at later stages of development.
Tobacco, alcohol, and cocaine are among the teratogenic drugs that can have harmful effects on the developing fetus. When pregnant women consume cocaine, it readily passes through the placenta and can lead to addiction in the fetus. This addiction is associated with a higher risk of fetal diseases and infant mortality. Cocaine use during pregnancy can result in various complications, including decreased birth weight, abnormalities, infarction of the cerebral cortex, and cardiovascular malformations.
Furthermore, the consumption of cocaine, marijuana, alcohol, tobacco, or heroin by pregnant women can increase the likelihood of premature birth. Cocaine specifically can induce premature labor through two mechanisms. Firstly, it causes vasoconstriction of blood vessels, leading to the premature separation of the placenta from the uterus by restricting blood flow. Secondly, it affects the contractility of the uterine myometrium, making it more responsive to signals that initiate labor.
It is worth noting that, except for muscle relaxants like succinylcholine and curare, most drugs used to induce labor can easily cross the placental membrane. Depending on the dosage and timing of administration in relation to labor, these drugs may cause respiratory depression in the newborn. As pregnancy progresses, the thinning of the placental membrane facilitates the passage of drugs.
The placenta is an extremely prolific producer of steroid and protein hormones, as well as prostaglandins. Two of its major products are steroid hormones: progesterone and estrogens, which are responsible for maintaining pregnancy and preventing spontaneous abortion and premature labor. Progesterone can be obtained from the placenta in all gestational stages, indicating that it is essential for maintaining pregnancy. The placenta forms progesterone from maternal cholesterol. A pregnant woman's ovaries can be removed after the first trimester without causing abortion, as progesterone is produced during the first weeks of pregnancy by the pregnancy corpus luteum in the ovary, but later (from the 11th week) it will be produced by the placenta, and the corpus luteum degenerates. Both progesterone and estrogens are produced in large quantities by syncytiotrophoblast.
Human chorionic gonadotropin (hCG), similar to luteinizing hormone (LH), is secreted for the first time by syncytiotrophoblast during the second week of pregnancy: it maintains the secretory activity of the corpus luteum, preventing the start of the next menstrual period. Its concentration is highest in fetal blood and urine at eight weeks, after which its concentration decreases.
The placenta is a prolific producer of steroid and protein hormones, as well as prostaglandins. Among its major products are steroid hormones, such as progesterone and estrogens. These hormones play a crucial role in maintaining pregnancy and preventing spontaneous abortion and premature labor. Progesterone, which is essential for sustaining pregnancy, can be obtained from the placenta throughout all stages of gestation. It is produced from maternal cholesterol. During the first trimester, progesterone is also produced by the pregnancy corpus luteum in the ovary. However, from the 11th week onwards, the placenta takes over progesterone production, leading to the degeneration of the corpus luteum. Syncytiotrophoblast, a component of the placenta, produces both progesterone and estrogens in large quantities.
In addition to steroid hormones, the placenta also synthesizes protein hormones through syncytiotrophoblast. One of these protein hormones is human chorionic gonadotropin (hCG), which is similar to luteinizing hormone (LH). Syncytiotrophoblast secretes hCG for the first time during the second week of pregnancy. This hormone helps maintain the secretory activity of the corpus luteum, preventing the onset of the next menstrual period. The concentration of hCG is highest in fetal blood and urine at eight weeks, after which it gradually decreases.
The production of hCG is exclusive to fetal tissue and is excreted in maternal urine, making it useful in pregnancy tests. However, it can also be abundantly produced by hydatidiform moles. If the hormone persists after two months of gestation, it may indicate a molar pregnancy.
In addition to hCG, the placenta produces various protein hormones such as human chorionic somatotropin (hCS) or human placental lactogen (hPL), human chorionic thyrotropin (hCT), human chorionic adrenocorticotropic hormone (hCACTH), insulin-like growth factors, corticotropin-releasing hormone, and endothelin. It is noteworthy that many of these hormones are also produced by the hypothalamus and pituitary gland.
Moreover, the placental membranes synthesize prostaglandins, a group of substances with multiple functions in different body tissues. Prostaglandins seem to play a crucial role in maintaining pregnancy and triggering labor. The initiation of labor appears to be signaled by a decrease in the progesterone to estrogen ratio, but the effect of this signal may be mediated by an increase in placental prostaglandin levels.
The placenta is an organ that develops during pregnancy and serves as a connection between the mother and fetus. It has two components: a fetal portion and a maternal portion. The placenta performs several functions, including protection, nutrition, respiration, excretion, and hormone production. It allows for the exchange of substances between the mother and fetus, such as nutrients, oxygen, and waste products.
Placental formation begins in the early weeks of pregnancy and reaches maturity by the end of the third month. The placenta consists of fetal villi that develop in an intervillous space filled with maternal blood. The villi exchange substances with maternal blood along the villous wall. The placenta also secretes hormones, including progesterone and estrogens, which are important for maintaining pregnancy.
The placenta is made up of various structures, including the intervillous space, placental septa, and the chorionic plate. Maternal blood enters the intervillous space through spiral arteries and circulates around the villous branches, allowing for nutrient and gas exchange. The fetal placental circulation involves the movement of blood from the fetus to the placenta through the umbilical arteries and back to the fetus through the umbilical vein.
The placenta has a discoidal shape and weighs approximately one-sixth of the fetal weight. It is expelled from the uterus after birth along with the fetal membranes.
The placenta can be affected by various factors, such as infections, teratogenic agents, and the Rh factor. Infections can cross the placenta and harm the fetus, while teratogenic agents can cause congenital abnormalities. The Rh factor can lead to complications if an Rh-negative mother carries an Rh-positive fetus.
The placenta also plays a role in hormone production, including progesterone, estrogens, and human chorionic gonadotropin (hCG). These hormones are important for maintaining pregnancy and supporting fetal development.
Overall, the placenta is a vital organ in pregnancy that facilitates the necessary exchanges between the mother and fetus for healthy development.
placenta, feto-maternal organ, transport mechanism, protection, nutrition, respiration, excretion, hormone production, placental formation, ovular element, fetal placenta, maternal element, maternal blood, intervillous space, fetal blood, villous vessels, nutritional substances, hormones, sex steroids, maternal antibodies, placental growth, decidua, blastocyst, endometrial stroma, placental development, chorion, villi, stem villi, terminal mesenchymal villi, intermediate mature villi, intermediate villi, terminal villi, placental villous tree, placental septa, cotyledons, placental expansion, chorionic villi, basal decidua, fetomaternal junction, cytotrophoblastic envelopes, maternal arteries, maternal veins, placental appearance, discoid shape, placental variations, placental dysfunction, choriocarcinoma, maternal surface, fetal surface, feto-placental circulation, umbilical arteries, arterio-capillary-venous system, maternal circulation, placental membrane, syncytiotrophoblast, cytotrophoblast, connective tissue, fetal capillaries, placental permeability, infectious agents, rubella virus, varicella-zoster virus, cytomegalovirus, Coxsackie virus, Treponema pallidum, human immunodeficiency virus (HIV), teratogenic agents, Rh factor, Rh-negative, Rh-positive, hemolytic disease of the newborn, placental barrier, teratogenic drugs, tobacco, alcohol, cocaine, placental endocrine secretion, steroid hormones, progesterone, estrogens, human chorionic gonadotropin (hCG), protein hormones, human chorionic somatotropin (hCS), human placental lactogen (hPL), human chorionic thyrotropin (hCT), human chorionic adrenocorticotropic hormone (hCACTH), insulin-like growth factors, corticotropin-releasing hormone, endothelin, prostaglandins.The Role of the Placenta in Fetal Development and Maternal HealthEmbryonic Support Structures I - The Placenta0000