The development of the respiratory system can be divided into two major stages. The first stage occurs between the third week and the sixth fetal month. It consists of two phases: the pseudoglandular phase and the canalicular phase. The pseudoglandular phase takes place between the fifth week and the fourth month and involves the differentiation of the bronchi and terminal bronchioles. The canalicular phase occurs between the fourth and sixth fetal months and involves the differentiation of the respiratory bronchioles and alveolar ducts. This stage is characterized by abundant vascularization.
The second stage occurs from the sixth fetal month until the age of 8. It is also divided into two phases: the terminal phase and the alveolar phase. The terminal phase occurs between the sixth month and birth and is marked by the appearance of the infundibula and primary alveoli. The alveolar phase extends from birth until the age of 7-8 years and involves the maturation and finalization of the alveoli. During this stage, the nasal cavity and nasopharynx acquire secondary specializations.
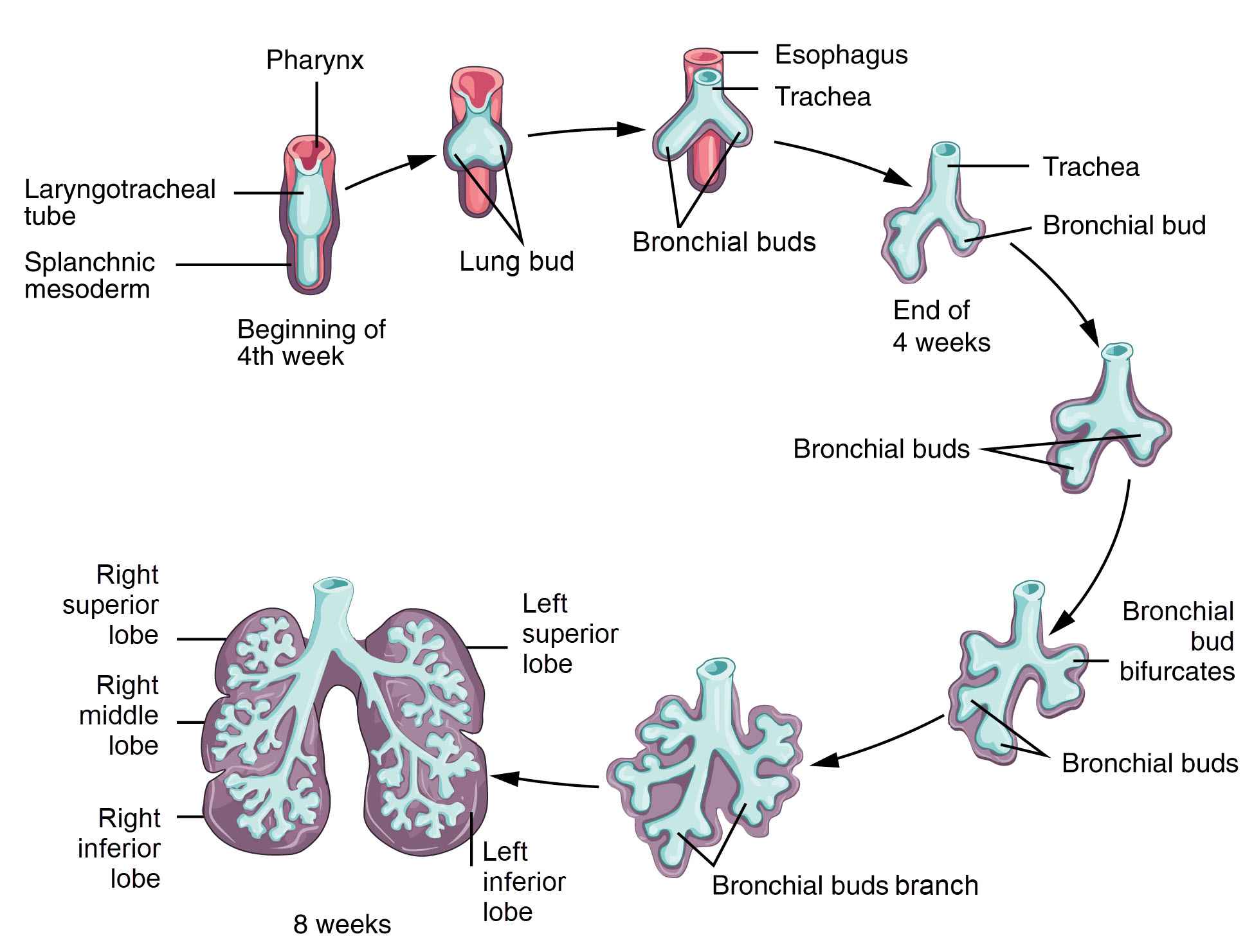
The formation of the pulmonary system begins with the appearance of a cavity called the respiratory diverticulum or pulmonary bud on day 22. This cavity is a diverticulum of the endoderm of the anterior intestine. In the third week, a circumscribed area is formed where endodermal cells multiply and proliferate, defining the pulmonary area. This area deepens into a pulmonary groove that transforms into a laryngotracheal canal (tube) and elongates over time. As the canal lengthens, two opposing folds are formed on the intestinal wall, which eventually unite into a mesenchymal wall called the tracheoesophageal septum. This septum separates the laryngotracheal canal from the anterior intestine between the fourth and seventh weeks, eventually forming the primordium for the esophagus. The lower segment of the laryngotracheal canal divides into two branches, each with a basal bud at its end. The lungs and bronchi develop from these basal buds. The larynx forms at the level of the upper segment of the laryngotracheal canal, while the trachea develops from the connecting piece towards the lower portion.
The respiratory system is formed from the ventral wall of the proenteron, and the epithelium of the larynx, trachea, bronchi, and pulmonary alveoli is of endodermal origin. The muscular, cartilaginous, and connective tissues of the respiratory system originate from the mesoderm.
The development of the lungs begins with the growth of the lung bud, which extends ventro-caudally through the mesenchyme surrounding the anterior intestine. Between days 22 and 28, the lung bud undergoes its first bifurcation, dividing into the right and left bronchial buds. These buds are the rudiments of the two lungs. From weeks 5 to 28, the bronchial buds continue to divide, forming the respiratory tree of the lung through 16 generations.
In the 7mm embryo, the lungs start to take shape as the primary bronchi begin to branch out. The right bronchus gives rise to two lateral branches: a small upper branch for the upper lobe of the lung and a middle branch for the middle lobe. The lower lobe is served by the caudal end of the primary bronchus. The left primary bronchus gives a single branch for the upper lobe and serves the lower lobe of the left lung. These branches continue to divide within the thickness of the dorsal mesocardium.
During the first bifurcation, the larynx and trachea start to form in the proximal part, while the primary bronchi (right and left) form in the proximal part of the second bifurcation. In the fifth week, a third round of branching occurs, resulting in the development of three secondary bronchial buds on the right side and two on the left side. These buds eventually develop into the pulmonary lobes.
In the sixth week, the fourth round of branching takes place, giving rise to 10 tertiary bronchi on the right side and 8 on the left side. These tertiary bronchi will become the bronchopulmonary segments of the mature lung.
Formation of lung primordia begins around the fourth week of development with the appearance of the respiratory diverticulum, also known as the lung bud. This bud emerges as an evagination of the ventral wall of the proenteron, the anterior intestine. The location of the bud within the intestinal tube is determined by the transcription factor TBX4, which is synthesized in the endodermal cells of the intestinal tube in the area where the respiratory diverticulum appears. TBX4 plays a crucial role in inducing the formation of the respiratory bud and promoting continuous growth and differentiation of the lungs.
The epithelium on the inner surface of the larynx, trachea, bronchi, and pulmonary epithelium are all derived from the endoderm. On the other hand, the muscular, cartilaginous, and connective tissue components of the trachea and lungs originate from the splanchnic mesoderm that surrounds the proenteron.
Initially, the lung bud freely communicates with the proenteron. However, as the diverticulum extends caudally, two longitudinal formations called the tracheo-esophageal ridges appear, separating it from the anterior intestine. Once these ridges fuse and form the tracheo-esophageal septum, the proenteron is divided into the esophagus (dorsal portion) and the trachea and lung buds (ventral portion). The respiratory primordium remains connected to the pharynx through the laryngeal opening.
During the fifth week of development, the lung primordia grow laterally and caudally, penetrating into the lumen of the pleuroperitoneal canals. This penetration forms the pulmonary prominences. As the transverse septum and stomach descend, the pleuroperitoneal canals elongate and become pleural cavities. The two layers of the pleural serosa, the visceral and parietal layers, develop from the mesothelium lining the walls of the canals. Fissures appear between the branches of each secondary bronchus, separating the pulmonary lobes. The right lung has two fissures, while the left lung has one. Additionally, on the mediastinal surface of the right lung, between the pericardium and diaphragm, the azygos lobe may develop due to excessive development of the second right ventral bronchus. However, the azygos lobe typically disappears in humans due to the bipedal position, which allows the lungs to expand during inspiration and increase respiratory capacity.
As development progresses, the lungs expand the pulmonary cavities, partially separating them from the heart and chest wall. The mediastinum, the space between the lungs, develops, and by the sixth week, the pericardial cavity separates from the pleural cavities.
Around the 16th week, the respiratory tree begins producing small branches known as terminal bronchioles. Between weeks 16 and 28, each terminal bronchiole further divides into two or more respiratory bronchioles after approximately 14 rounds of branching. During this period, the mesodermal tissue surrounding these structures becomes highly vascularized.
Around the 16th week, the respiratory tree begins producing small branches known as terminal bronchioles. Between weeks 16 and 28, each terminal bronchiole further divides into two or more respiratory bronchioles after approximately 14 rounds of branching. During this period, the mesodermal tissue surrounding these structures becomes highly vascularized said in the beginning, during the development of the lungs, there are four phases that take place. The first phase is the pseudoglandular phase, where the lungs have a glandular appearance and the bronchial tree epithelium is cuboidal. Following this is the canalicular phase, where terminal sacs composed of flat cells appear, allowing for respiration. The third phase is the terminal sac phase, during which cells that regulate the surface tension of the respiratory membrane and secrete surfactant develop. The absence of these cells can lead to the development of hyaline membrane disease, causing respiratory distress syndrome. This phase is also marked by the strong development of the lymphatic network. The final phase, known as the alveolar phase, occurs around the age of 7-8 years.
Starting from week 28, the respiratory bronchioles begin to produce a final generation of short bronchi. By week 36, the newly formed branches of the terminal bronchioles are surrounded by a network of capillaries and are referred to as terminal sacs or primitive alveoli. At this stage, limited breathing is possible, although the alveoli are still few and immature. Unfortunately, babies born during this period often succumb to respiratory failure.
During lung maturation, bronchioles continue to divide until the seventh month of intrauterine life. This results in the formation of smaller channels during the canalicular period. Simultaneously, the vascular supply to the lungs increases steadily. The process of respiration begins after the pseudoglandular phase and the canalicular phase, which occur between weeks 5-16 and weeks 16-26 respectively. During this time, the cuboidal cells of the respiratory bronchioles transform into thin, flattened cells. These cells are closely associated with numerous blood and lymphatic capillaries, creating spaces known as terminal sacs or primitive alveoli. By the seventh month, enough capillaries have developed in each lung to facilitate gas exchange and support the survival of premature newborns.
In the last two months of prenatal life and for several years after birth, the number of terminal sacs gradually increases. The cells lining the inner surface of the terminal sacs, referred to as type I alveolar epithelial cells, flatten in a way that allows the surrounding capillaries to protrude into the alveolar sacs. This close contact between the epithelial cells and endothelial cells forms the alveolar-capillary membrane. Mature alveoli appear after birth. Additionally, at the end of the sixth month, type II alveolar epithelial cells develop and produce surfactant. Surfactant is a phospholipid-rich fluid that reduces surface tension at the interface between air and alveolar membranes.
Before birth, the lungs are filled with a fluid that contains a high concentration of chloride, small amounts of proteins, mucus synthesized by bronchial glands, and surfactant synthesized by type II alveolar epithelial cells. The amount of surfactant in this fluid increases, particularly in the last two weeks before birth. This surfactant forms a phospholipid layer on the alveolar membranes.
Fetal respiratory movements play a crucial role in the development of the lungs and respiratory muscles. These movements begin before birth and stimulate the aspiration of amniotic fluid. When breathing is initiated at birth, the majority of the fluid in the lungs is quickly absorbed into the blood and lymphatic capillaries. A small amount may be eliminated through the bronchi and trachea during birth. Surfactant, a thin layer of phospholipids, remains on the cell membranes of the alveoli after absorption. During the first breath, surfactant prevents the formation of high surface tension at the air-water (blood) interface, thus preventing alveolar collapse during expiration. The absence or reduced presence of surfactant in premature newborns leads to respiratory distress syndrome (RDS) and the collapse of primitive alveoli (hyaline membrane disease).
Before birth, each lung forms 20-70 million terminal sacs. These sacs continue to form and differentiate in a cranio-caudal progression before and after birth until the age of 8.
After birth, air enters the lungs through respiratory movements, causing the lungs to expand and fill the pleural cavities. The growth of the lungs after birth is primarily due to an increase in the number of respiratory bronchioles and alveoli, as well as an increase in the size of the pulmonary alveoli. The process of forming new alveoli continues throughout the first 10 years of postnatal life, resulting in only one-sixth of the number of alveoli present at birth compared to an adult. The mature lung contains a total of 300-400 million terminal sacs.
The development of the larynx has a dual origin. The supraglottic region develops from the ventral wall of the primitive pharynx, while the subglottic region develops from the cranial end of the laryngotracheal diverticulum. At the 5mm embryo stage, which is around the fourth week of development, the embryonic larynx resembles the larynx of adult fish with air breathing. It has two mobile folds on the sides of the communication site between the laryngotracheal tube and the pharynx. These folds will become the vocal folds, and the space between them will become the glottis. To protect these structures, new elements differentiate, including the epiglottis, the aryepiglottic folds, the pharyngoepiglottic folds, the glosoepiglottic folds, and the ventricular folds.
The cartilages and muscles of the larynx originate from the mesenchyme of the fourth, fifth, and sixth pharyngeal arches, while the inner layer is of endodermal origin.
The laryngeal primordium consists of two arytenoid outgrowths and an epiglottic outgrowth. The epiglottic outgrowth is located posterior to the copula, which will transform into the root of the tongue. The epiglottic outgrowth has two marginal portions that will develop into aryepiglottic folds.
Due to the rapid growth of the arytenoid outgrowths, the interior space of the larynx becomes smaller and forms a slit. This slit will temporarily close during the second month through the proliferation of epithelial cells. After some of these cells regress and the laryngeal primordium elongates, the internal cavity of the larynx (cavitas laryngis) appears. Within this cavity, the cranial part differentiates into the epiglottic folds, and the caudal part differentiates into the vocal folds. In terms of cartilage development, a primordium of an annular cartilage can be observed in the third month, derived from the first tracheal arch. This is followed by the paired primordia of the thyroid cartilage, derived from the fourth and fifth branchial arches, which later fuse. The fixed cartilages then form in the arytenoid outgrowths, and in the fifth month, the definitive epiglottis forms from the epiglottic primordium.
The rapid proliferation of mesenchyme in the laryngeal orifice causes a change in its sagittal aspect, resulting in a T-shaped opening. As the mesenchyme from the two pharyngeal arches transforms into the thyroid, cricoid, and arytenoid cartilages, the laryngeal orifice takes on the characteristic shape found in adults.
During the formation of the cartilages, the laryngeal epithelium undergoes rapid proliferation, temporarily obstructing the lumen. This leads to the formation of laryngeal ventricles, which are a pair of lateral recesses. Vacuolization and repermeabilization occur, and fold tissues differentiate to form both the false and true vocal cords.
The laryngeal muscles receive innervation from branches of the cranial nerve X (vagus) because they are derived from the mesenchyme of the fourth and sixth pharyngeal arches. The superior laryngeal nerve innervates structures derived from the fourth laryngeal arch, while the recurrent laryngeal nerve innervates structures derived from the sixth pharyngeal arch. In the fetus and newborn, the larynx is positioned high, but it descends during childhood and adolescence. It reaches its final, adult position during puberty.
The formation of the trachea and bronchi begins with the bifurcation of the tracheobronchial diverticulum in the 4 mm embryo, at three weeks. At this stage, the right branch extends vertically, while the segment between the bifurcation site and the origin elongates to become the trachea. The differentiation of the tracheal and bronchial glands occurs in the fifth fetal month, and the smooth musculature and semicartilaginous rings form in the seventh fetal week.
The pulmonary bud separates from the proenteron and gives rise to the trachea and two lateral prominences known as bronchial buds. These buds grow in size during the fifth week and develop into the right and left main bronchi. From the right main bronchus, three secondary bronchi form, while the left main bronchus gives rise to two secondary bronchi, indicating the formation of three pulmonary lobes on the right side and two lobes on the left side. An abnormal division of the proenteron by the tracheoesophageal septum can lead to tracheoesophageal fistulas and esophageal atresia.
Initially, the trachea is a short epithelial tube. In the fourth week, cartilaginous rings begin to form within the mesenchyme, which fully develop into cartilage during the seventh and eighth weeks. The smooth musculature and blood vessels also originate from the visceropleural mesenchyme. Tracheal glands develop from epithelial buds in the early fourth month.
As the lung buds grow caudally and laterally, they increase in volume, causing the pericardio-peritoneal canals to narrow down. These canals are located on each side of the proenteron and gradually become occupied by the developing lung buds. The pleuro-peritoneal and pleuro-pericardial folds separate the pericardio-peritoneal canals from the peritoneal and pericardial cavities, creating primitive pleural cavities. The visceral pleura, derived from the mesoderm covering the outer surface of the lungs, develops alongside the parietal pleura, which covers the inner surface of the trunk wall. The space between the parietal pleura and the visceral pleura forms the pleural cavity.
The development of the bronchial tree and alveolar system begins with the basal buds located at the end of the laryngotracheal tube. These buds divide into three daughter buds on the right side and two daughter buds on the left side. These daughter buds develop into vesicles connected by a stalk, which form the primordia for the lung lobes. Through successive divisions, the pulmonary subunits are formed, including segments, subsegments, and alveoli. The inner lining of the bronchi develops from the epithelial ducts, while the surrounding mesenchyme gives rise to the cartilages, smooth muscles, and blood vessels.
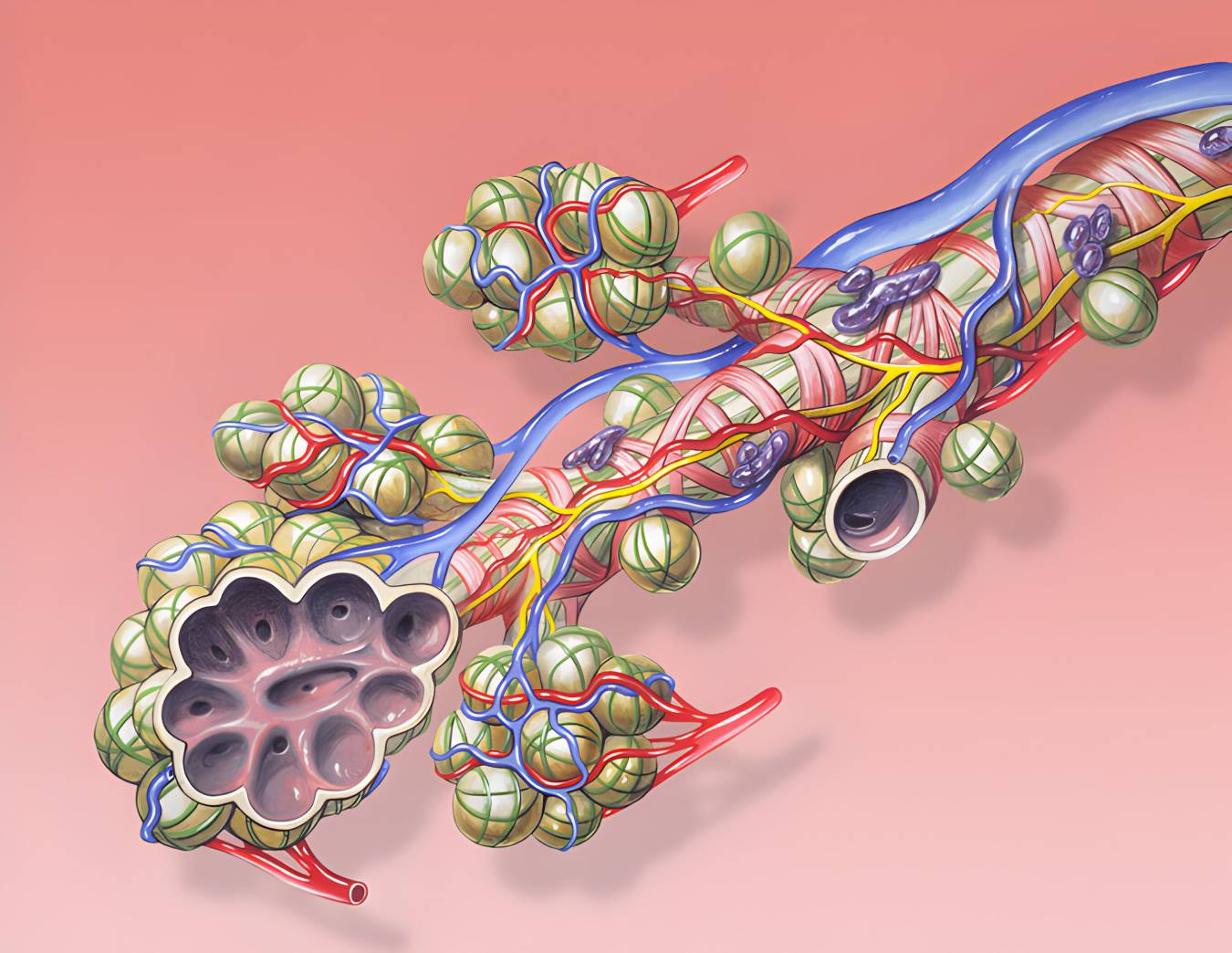
As the lung buds grow, the pericardio-peritoneal canals narrow and the bronchi expand. The peripheral epithelium becomes more flattened, and formations called pulmonary alveoli appear at the terminal segments of the lung primordium. These alveoli are initially lined with capillaries, and the cuboidal epithelium flattens, allowing neighboring capillaries to surround the flat epithelium. This vascularization and the presence of surfactant inside the alveoli enable premature newborns after the seventh month to survive at birth.
The secondary bronchi divide in a dichotomous manner, giving rise to 10 tertiary bronchi in the right lung and 8 in the left lung, forming the bronchopulmonary segments in adults. By the end of the sixth month, approximately 17 generations of subdivisions are formed, and six additional divisions occur in the postnatal period.
The branching process is controlled by interactions between the endoderm of the lung bud and the surrounding splanchnic mesoderm. The mesodermal cells emit signals, including members of the fibroblast growth factor family, that induce branching. The development of the bronchial tree leads to the lungs being positioned more caudally, and at birth, the trachea bifurcates at the level of the fourth thoracic vertebra.
Developmental anomalies of the lungs can range from severe conditions like pulmonary agenesis to defects in pulmonary branching and subdivision of terminal respiratory bronchioles.
Pulmonary agenesis is the most severe anomaly where the pulmonary bud fails to divide into the right and left bronchi, resulting in no growth. It can either manifest as bilateral or unilateral agenesis.
During the embryonic and fetal periods, defects in pulmonary branching can lead to abnormalities in the number of pulmonary lobes or segments, and in some cases, the complete absence of a lung. On the other hand, defects in the subdivision of terminal respiratory bronchioles can cause a decrease in the number of alveoli, even if the rest of the respiratory tree is normal.
Overall, pulmonary hypoplasia, which is characterized by a reduced number of pulmonary segments or terminal air sacs, is a response to various factors that reduce the volume of the pleural cavity. This reduction in volume hinders lung growth.
At the level of the lungs, there can be: unilateral or bilateral agenesis due to the lack of development of the pulmonary buds; pulmonary hypoplasia accompanied by posterolateral diaphragmatic hernia; variation in the number of lobes, such as the presence of the left middle lobe or the azygos lobe in the right lung; ectopic lung lobes developed from the trachea or esophagus; congenital pulmonary cysts.
At the level of the larynx, atresia or absence of the epiglottis can be observed. The occurrence of esophagotracheal fistulas due to a posterior median fissure of the cricoid cartilage, either an atretic and transversely divided esophagus. There can be: tracheal atresia, tracheal deformities, and diverticula.
The development of the respiratory system can be divided into two major stages. The first stage occurs between the third week and the sixth fetal month and consists of the pseudoglandular phase and the canalicular phase. The pseudoglandular phase involves the differentiation of the bronchi and terminal bronchioles, while the canalicular phase involves the differentiation of the respiratory bronchioles and alveolar ducts. The second stage occurs from the sixth fetal month until the age of 8 and includes the terminal phase and the alveolar phase. The terminal phase is marked by the appearance of the infundibula and primary alveoli, while the alveolar phase involves the maturation and finalization of the alveoli.
The development of the lungs begins with the growth of the lung bud, which divides into the right and left bronchial buds. From weeks 5 to 28, the bronchial buds continue to divide, forming the respiratory tree of the lung through 16 generations. The branching process occurs in several rounds, resulting in the development of secondary and tertiary bronchi, which eventually form the bronchopulmonary segments of the mature lung.
The development of the respiratory system is regulated by various factors, including transcription factors and signaling molecules. The epithelium of the respiratory system is of endodermal origin, while the muscular, cartilaginous, and connective tissues originate from the mesoderm.
During lung maturation, there are four phases: the pseudoglandular phase, the canalicular phase, the terminal sac phase, and the alveolar phase. Each phase is characterized by specific changes in the lung structure and function.
The formation of the larynx and trachea involves the differentiation of various structures, including the vocal folds, epiglottis, and cartilages. The laryngeal muscles receive innervation from the cranial nerve X (vagus). The formation of the trachea and bronchi begins with the bifurcation of the tracheobronchial diverticulum, and subsequent branching leads to the formation of the bronchial tree and alveolar system.
Developmental anomalies of the lungs can range from severe conditions like pulmonary agenesis to defects in pulmonary branching and subdivision of terminal respiratory bronchioles. Pulmonary hypoplasia, characterized by a reduced number of pulmonary segments or terminal air sacs, can occur due to various factors that reduce the volume of the pleural cavity.
Overall, the development of the respiratory system is a complex process that involves the differentiation and maturation of various structures, and any disruptions in this process can lead to developmental anomalies.
respiratory system, development, stages, pseudoglandular phase, canalicular phase, terminal phase, alveolar phase, respiratory diverticulum, pulmonary bud, endoderm, mesoderm, lung buds, bronchial buds, respiratory tree, bronchial branching, trachea, larynx, pulmonary lobes, alveoli, surfactant, respiratory distress syndrome, fetal development, terminal bronchioles, alveolar-capillary membrane, lung maturation, gas exchange, pleural cavities, respiratory movements, laryngeal development, tracheobronchial diverticulum, bronchial tree, alveolar system, developmental anomalies, pulmonary agenesis, pulmonary hypoplasia, lung lobes, congenital pulmonary cysts, laryngeal anomalies, esophagotracheal fistulas, tracheal atresia, tracheal deformities, diverticulaThe Stages and Anomalies of Lung and Larynx DevelopmentThe Development of the Respiratory System0000