During fetal life, the process of oocyte development begins and is discontinuous. The ovaries start producing primary oocytes from the fifth month of intrauterine development. Female germ cells undergo mitotic divisions and differentiate into oogonia, surrounded by cells of the sex cords. From the 12th week of development, millions of oogonia enter the prophase of the first meiosis and remain in a latent stage. The nucleus of these primary oocytes contains partially condensed chromosomes and is called the germinal vesicle. The primary oocytes are enclosed by a capsule formed by follicular epithelial cells, creating a primordial follicle.
The flat follicular cells secrete an oocyte maturation inhibitor factor, which protects the oocyte from environmental influences. In the fifth month of development, there are approximately 7 million primordial follicles, but most of them degenerate. At birth, there are only 700,000 - 2,000,000 primordial follicles remaining, and this number decreases to 40,000 at puberty. Throughout a woman's reproductive life, only 400 - 500 oocytes will be ovulated. The menstrual cycle, controlled by female hormonal cycle (hypothalamic, pituitary, and ovarian hormones), regulates folliculogenesis, ovulation, and the state of the uterine mucosa.
Around the fifth day after menstruation begins, the hypothalamus secretes a hormone called GnRH, which stimulates the pituitary to secrete luteinizing hormone (LH) and follicle-stimulating hormone (FSH). This initiates the first menstrual cycle in female puberty (menarche) and the folliculogenesis in the ovary. Under the influence of FSH, the follicular epithelium cells increase in volume and change shape, becoming cuboidal. These primary follicles multiply and form multiple layers of granulosa cells. The granulosa cells are separated from the ovarian stromal cells by a basal membrane. The follicles also develop an internal sheath and an external sheath, both vascularized.
The follicular cells and the oocyte secrete a glycoprotein material called the zona pellucida, which forms a physical barrier between the follicular cells and the oocyte. Thin extensions of the follicular cells, called digitations, remain connected to the oocyte's cell membrane through junctions. Some follicles degenerate, while others continue to enlarge and form a central fluid-filled cavity called the antrum. These follicles are known as secondary follicles. Only one follicle becomes dominant and continues to enlarge, while the others degenerate. The oocyte progresses within the developing antrum, surrounded by a mass of follicular cells called cumulus oophorus. The dominant follicle, known as the Graafian follicle, is mature but the oocyte has not completed meiosis.
The reason for the limited number of primordial follicles that initiate folliculogenesis each month, as well as the selection of only one follicle to mature, remains unknown. One theory proposes that as follicles progress in development, they become more sensitive to the stimulating effects of FSH. This would result in the more advanced follicles to FSH and being favored. Another theory suggests that the selection process is controlled by a complex feedback system involving pituitary and ovarian hormones and growth factors.
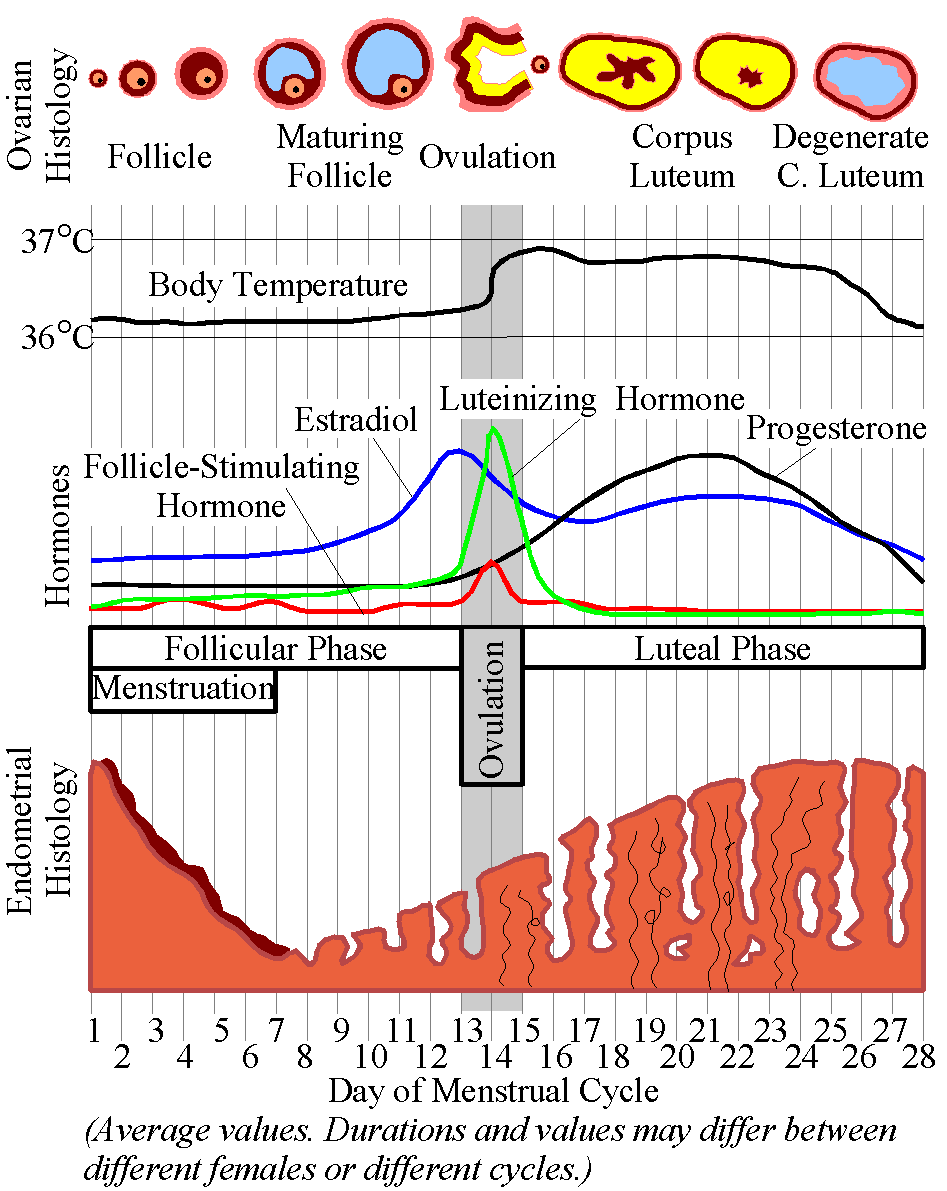
On the 13th-14th day of the menstrual cycle, which marks the end of the proliferative phase of the uterine endometrium, the levels of pituitary gonadotropin hormones (LH and FSH) increase abruptly. These increases stimulate the primary oocyte of the remaining mature Graafian follicle to complete its meiosis. This occurs approximately 15 hours after the rise in LH and FSH levels, causing the bulging germinal vesicle membrane of the oocyte to rupture. After 20 hours, the chromosomes align in metaphase, and cell division occurs to form the secondary oocyte and the first polar body. The secondary oocyte then begins the second meiotic division but enters meiotic arrest about 3 hours before ovulation.
In response to the increase in LH and FSH, the cumulus oophorus expands, and the intercellular connections of the cumulus cells surrounding the oocyte are lost. This leads to their disintegration, causing the oocyte to detach into the antral cavity while surrounded by a detached mass of cumulus cells. The dispersal of cumulus cells is influenced by the hyaluronic acid secreted by them. Additionally, an abundant extracellular matrix is formed, which may play a role in various processes, including the regulation of meiosis and ovulation. Furthermore, this matrix mass and the cumulus cells accompanying the ovulated oocyte may contribute to the transport of the oocyte into the oviduct, fertilization, and the early stages of zygote development.
Ovulation, the process of the secondary oocyte being expelled from the follicle, appears to have similarities to an inflammatory response. The events leading up to ovulation are believed to be triggered by the release of histamine and prostaglandins, which are well-known inflammatory mediators. Following an increase in FSH and LH, the follicle becomes more vascularized, pink, and edematous compared to non-developed follicles. It moves towards the surface of the ovary and forms a prominence known as the stigma. As ovulation approaches, the follicle wall becomes thinner and forms a small nipple-like prominence. Eventually, the tension from smooth muscle cells in the follicular wall, along with the release of enzymes that degrade collagen and other factors, causes the follicle to rupture. This rupture is not explosive, and the oocyte, along with cumulus cells, is slowly released onto the surface of the ovary.
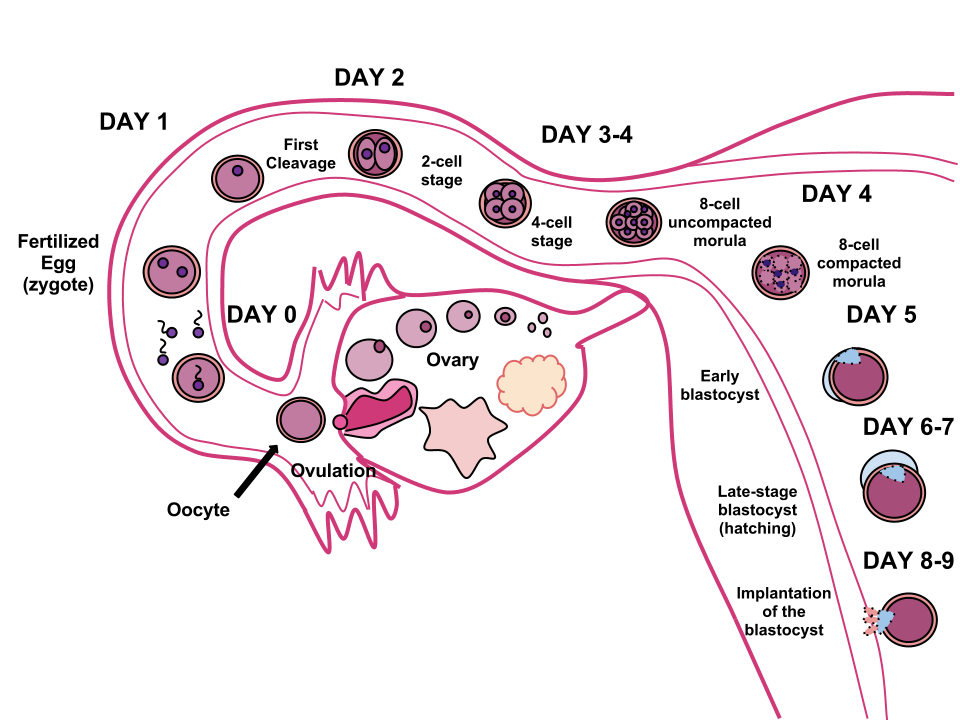
Ovulation typically occurs around 38 hours after FSH and LH growth begins. The oocyte, along with the cumulus oophorus, is then transported to the fallopian tube's ampulla through synchronized movements of cilia in the fallopian tube wall. Inside the ampulla, the oocyte remains viable for 24 hours before losing its ability to be fertilized. The ruptured follicle transforms into the endocrine corpus luteum. After ovulation, the granulosa cells of the follicle multiply and give rise to the luteal cells of the corpus luteum. This structure secretes steroid hormones that prepare the uterine endometrium to receive an embryo. If the embryo does not implant, the corpus luteum degenerates after approximately 14 days, becoming the corpus albicans.
During follicular development, under the influence of FSH, a number of 5-15 primordial follicles begin to develop. However, only one follicle reaches maturity and releases one oocyte during ovulation under normal conditions. In the initial phase of follicular development, a large number of follicular and thecal cells secrete estrogen, starting from the 5th day of the menstrual cycle. This estrogen stimulates the proliferation of the endometrium, leading to the proliferative phase of endometrial differentiation, which begins on the 5th day and is complete on the 9th day.
After ovulation, the thecal cells in the corpus luteum continue to secrete estrogen, while the luteal cells secrete progesterone. Progesterone stimulates the proliferation of the endometrium, the formation of glandular structures, and an increase in vascularization, resulting in the secretory phase of endometrial differentiation. If the embryo does not implant towards the end of the menstrual cycle, the corpus luteum shrinks, causing a decrease in progesterone levels. This leads to the degeneration and shedding of the dependent endometrium during the menstrual phase, which typically lasts 4-5 days and includes the elimination of the endometrium, unfertilized oocyte, and approximately 35 ml of blood.
Some women may experience mild pain during ovulation, which occurs around the middle of the menstrual cycle. Additionally, there is a slight increase in temperature (approximately 0.3 °C) during ovulation, which can be monitored to determine the timing of oocyte release.
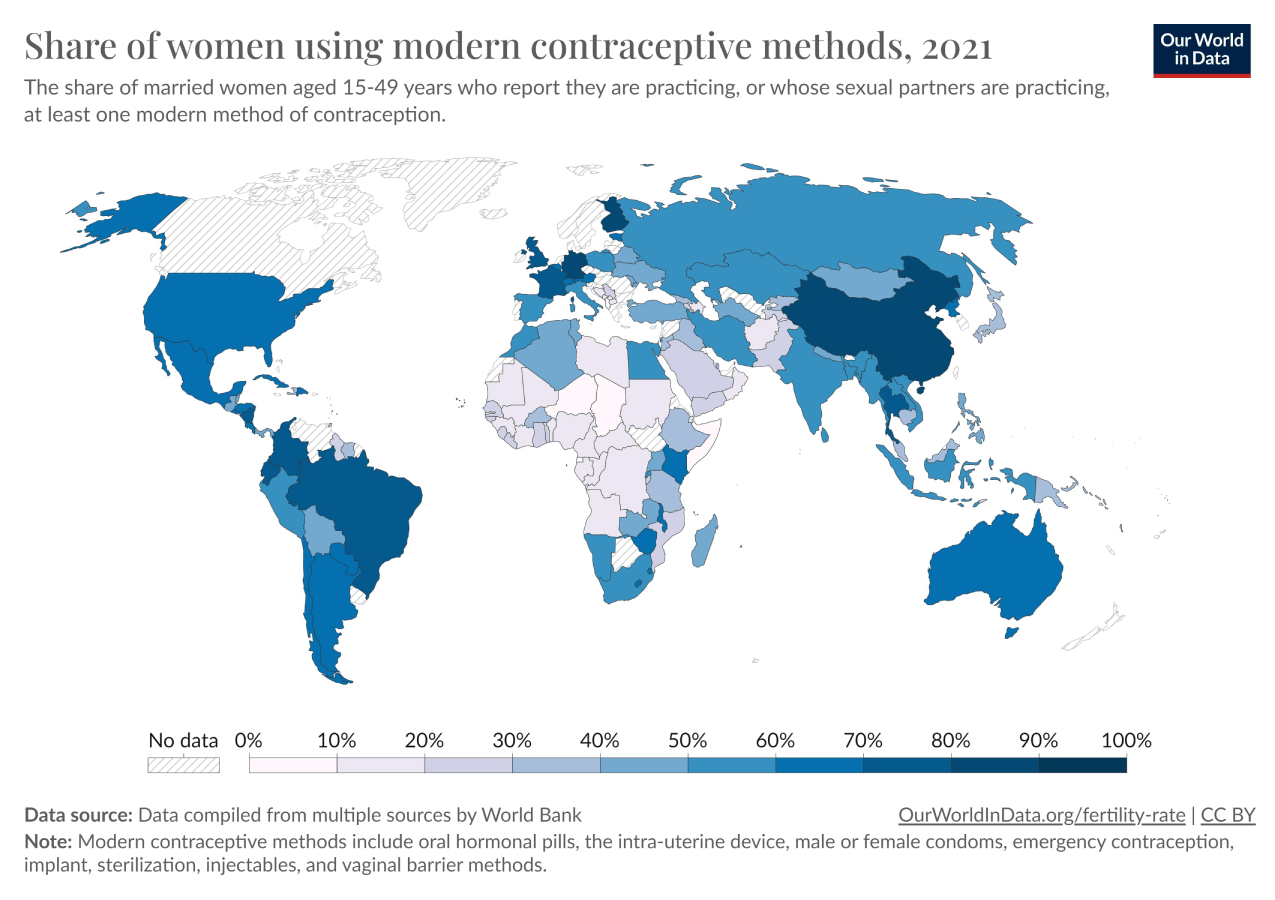
Ovulation can be inhibited by administering progesterone components orally from the 5th day to the 25th day of the menstrual cycle. This acts as a contraceptive by inhibiting ovulation in almost all cases. Anti-ovulatory preparations also contain a low amount of estrogen alongside progesterone. The estrogen component prevents ovulation, while the progesterone component ensures a normal menstrual bleeding after discontinuing contraceptive medication on the 25th day of the cycle.
During fetal development, the ovaries start producing primary oocytes, which remain in a latent stage. At birth, there are only a few hundred thousand primordial follicles remaining, and this number decreases to around 40,000 at puberty. Throughout a woman's reproductive life, only a few hundred oocytes will be ovulated. The menstrual cycle, controlled by hormones, regulates folliculogenesis, ovulation, and the state of the uterine mucosa.
The menstrual cycle begins with the secretion of GnRH by the hypothalamus, which stimulates the pituitary to release LH and FSH. FSH initiates folliculogenesis in the ovary, leading to the development of primary follicles. One follicle becomes dominant and continues to grow, while the others degenerate. The dominant follicle, known as the Graafian follicle, contains a mature oocyte. The levels of LH and FSH increase, causing the oocyte to complete its meiosis and rupture from the follicle.
Ovulation occurs around 38 hours after the increase in LH and FSH levels. The oocyte is transported to the fallopian tube and remains viable for 24 hours. The ruptured follicle transforms into the corpus luteum, which secretes hormones to prepare the uterine endometrium for embryo implantation. If the embryo does not implant, the corpus luteum degenerates, leading to the shedding of the endometrium during menstruation.
Ovulation can be inhibited by administering progesterone components, which act as contraceptives by inhibiting ovulation.
fetal development, ovaries, primary oocytes, latent stage, birth, primordial follicles, puberty, reproductive life, ovulated, menstrual cycle, hormones, folliculogenesis, ovulation, uterine mucosa, GnRH, hypothalamus, pituitary, LH, FSH, follicle, Graafian follicle, mature oocyte, meiosis, rupture, fallopian tube, corpus luteum, hormones, uterine endometrium, embryo implantation, degenerates, shedding, menstruation, progesterone components, contraceptives, inhibiting ovulation, ovum.The Menstrual Cycle and Ovocyte Development: From Folliculogenesis to Ovulation and BeyondGametogenesis III - Ovogenesis0000