When evaluating patients with suspected pulmonary embolism (PE), the PESI and sPESI scores provide valuable tools to assess the severity of the condition and guide treatment decisions. These scores help identify high-risk patients who may require more aggressive intervention and guide appropriate management strategies. Let's delve into their application:
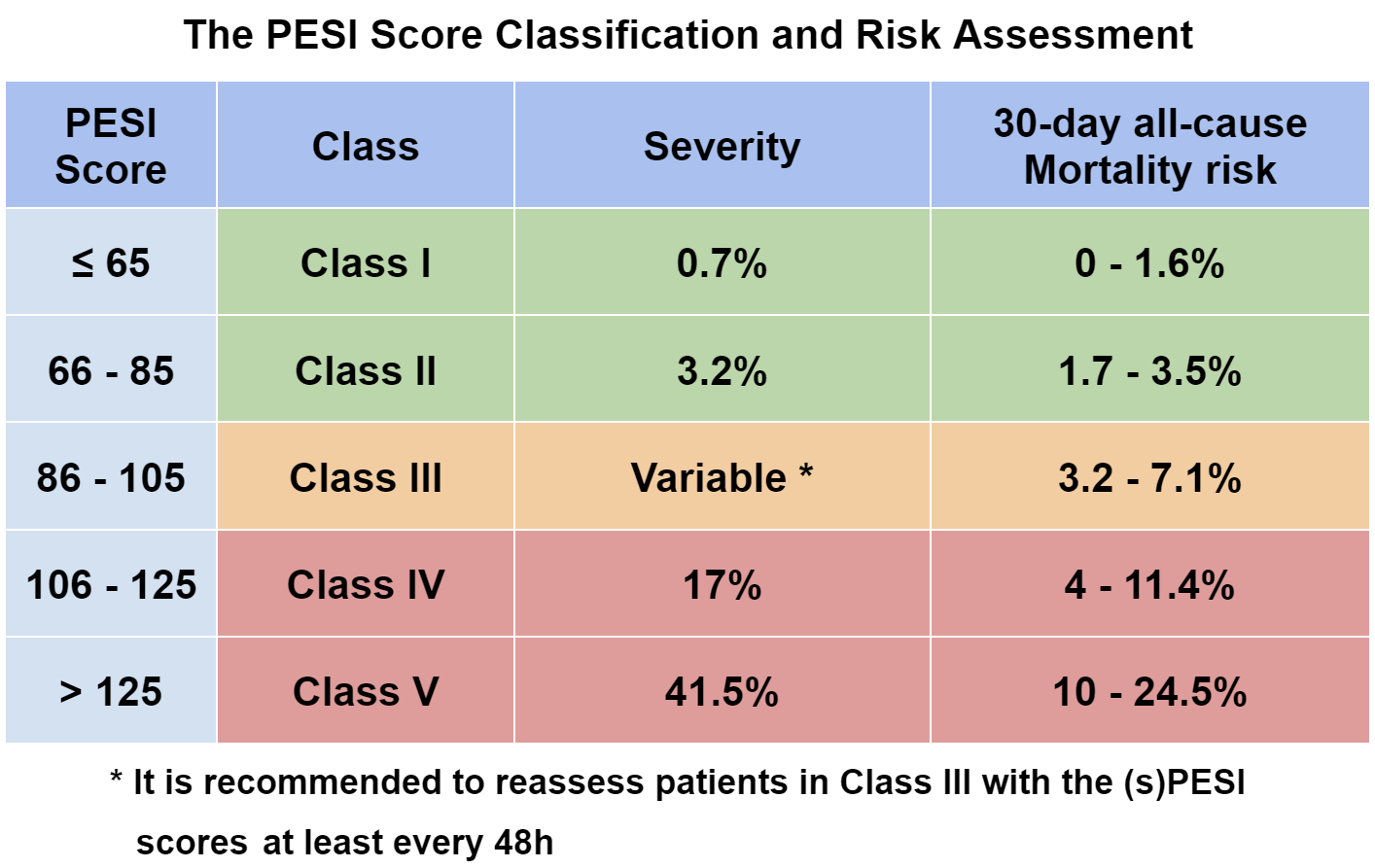
The PESI (Pulmonary Embolism Severity Index) score is a widely recognized risk assessment tool that considers various clinical factors to classify patients into different risk classes. A higher PESI score indicates a more severe condition and a higher risk of adverse outcomes. Based on a meta-analysis of 21 studies, a higher PESI score has been associated with increased PE-related mortality, all-cause mortality, and serious adverse events[1].
The sPESI (simplified Pulmonary Embolism Severity Index) score is a simplified version of the PESI score, designed for easier and quicker use. While maintaining a similar predictive capacity, the sPESI score offers the advantage of simplicity and efficiency[1]. It has been shown to have comparable odds ratios for PE-related mortality, all-cause mortality, and serious adverse events as the PESI score[1].
Initial Assessment: Both the PESI and sPESI scores can help clinicians initially classify patients into risk categories upon presentation. Patients with higher scores may require closer monitoring, aggressive treatment, or hospitalization[2].
Subsequent Evaluation: It's important to recognize that subsequent evaluations are crucial in refining risk assessment. Patients initially classified as high-risk may be re-evaluated to potentially downgrade their risk level. For instance, a study showed that patients in the third PESI class who were reclassified to lower classes after 48 hours had significantly lower average mortality[4].
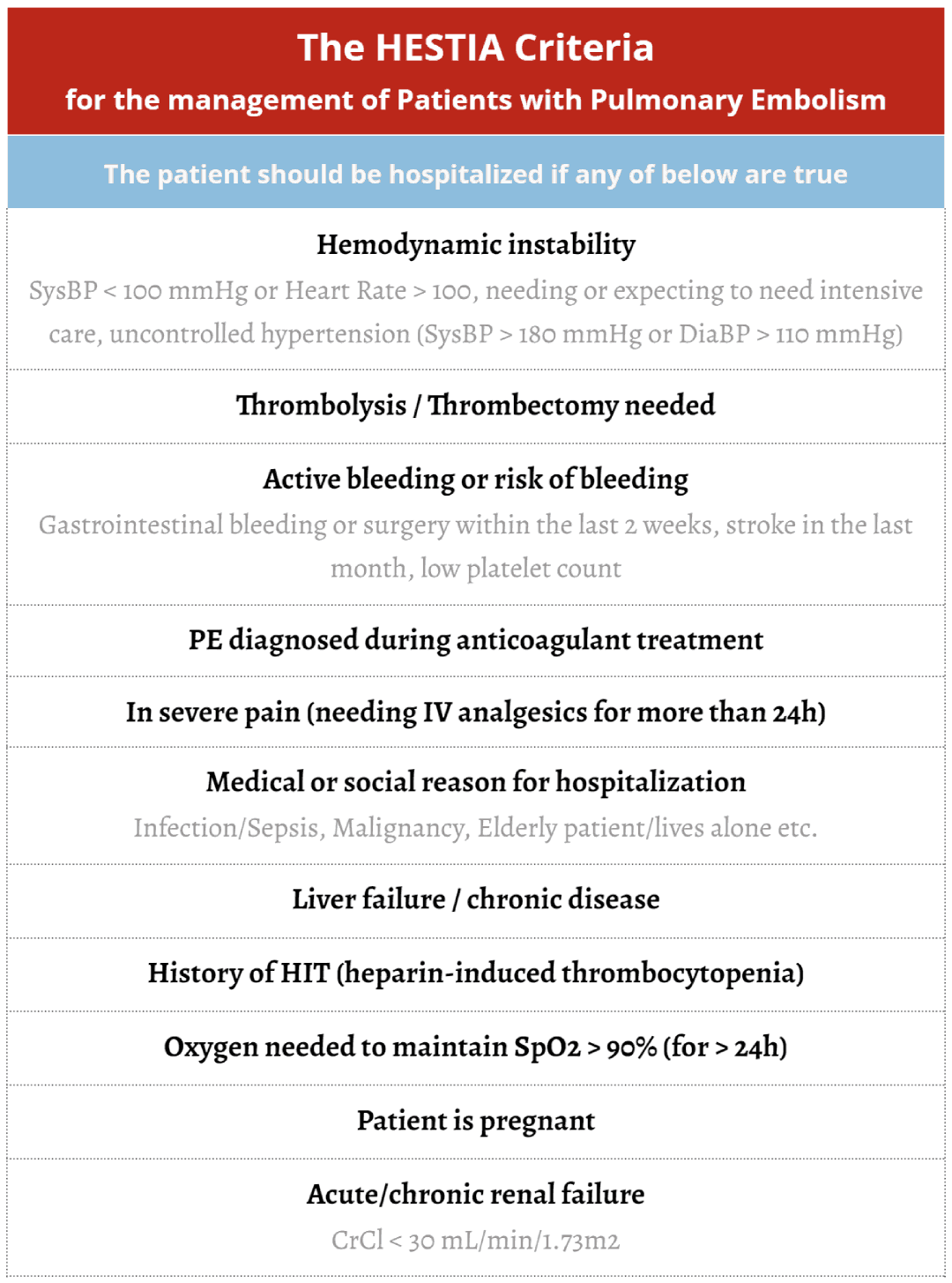
Patient Management: The PESI score aids in identifying low-risk patients who could potentially be managed as outpatients, considering factors such as the HESTIA Criteria[3]. The sPESI score, while slightly more variable, remains a practical tool for assessing mortality risk when multiple assessments are necessary[1].
Incorporating statistical data, a study found that the PESI score accurately identified 35% of low-risk PE patients, highlighting its clinical utility[4]. Additionally, a post-hoc analysis revealed that a significant portion of PE patients (46%) could be safely treated at home, emphasizing the role of risk assessment in determining appropriate treatment settings[3].
In summary, the PESI and sPESI scores offer valuable insights into the severity of pulmonary embolism, aiding healthcare professionals in risk assessment and patient management. While the PESI score provides comprehensive risk classification, the sPESI score offers a simpler alternative without compromising predictive accuracy. Regular evaluations and consideration of patient-specific factors further enhance risk assessment precision and inform optimal care decisions.
A meta-analysis of 21 studies demonstrated that a higher PESI score was significantly associated with a higher PE related-mortality (OR of 11.1), a higher all-cause mortality (OR of 7.7), and with serious adverse events (OR of 2.94). [1] The sPESI score had a similar OR for all three events: OR of 11.1 for PE-related mortality, 12.5 for all-cause mortality, and 3.33 for serious adverse events. Although from the data it seems that the sPESI score is even more fit for tracking mortality risk (higher AUC), it had higher variability between cases. Still, sPESI is much easier to use and is sufficient for mortality estimation if multiple assessments are necessary. [1], [2]
Some specialists prefer assessing patient risk with the PESI score at presentation, and with the sPESI score during hospitalization, due to its ease of use.
Another study done in 2005 on america patients hospitalized during the 1990s and 2000s noted that tried doing an analysis on incidence of DVT & PE and found the following: [2]
One study done in 2013 showed that the PESI score was able to accurately identify that 35% of patients with PE were low-risk, while noting that some high-risk patients might still be treated in the outpatient environment (please refer to the HESTIA Criteria chart for more help deciding what the appropriate management is). [3], [4], [5]
Out of the 4,713 patients, 1,136 had an objective diagnosis of PE and 1,097 could be accurately assessed retrospectively. These patients were further risk-stratified with the help of the PESI score in the following manner: 13.5% were classified as class I, 21.3% as class II, 19.4% as class III, 21.3% as class IV, and 17.8% as class V.
The patients noted that out of all patients (307) classified in the third category, 3 died in the first 48h after diagnosis. Of the remaining 304, 83 (27.3%) were further reclassified into lower classes on subsequent evaluations after 48h, and these had a much lower average mortality (1.2%) than the rest that couldn't be reclassified (11.3%). 16 patients were re-classified into the 4th group, and these patients had a mortality of 50%. Average mortality of the patients into the 3rd group was 8.3%. [4]
The study aims to demonstrate that while the initial PESI score is able to accurately identify high-risk patients, subsequent evaluations are equally important to further assess mortality risk and better adapt patient management. [4] In patients belonging to groups I-III, the Hestia criteria is an important tool for not only deciding whether to hospitalize a patient, but to further assess risk profile in some patients. [5]
Another study doing a post-hoc analysis of the YEARS study found out that: [3], [6]
The sPESI score proves its value in predicting short-term outcomes for pulmonary embolism (PE) patients. Patients with a sPESI score of 0, comprising 22% of cases (data from a study done in 2018 on 1715 patients from the COMMAND VITE Registry - a japanese Thromboembolism patient database -), exhibited low 30-day mortality (6.4%) and reduced cumulative incidence of mortality, recurrent venous thromboembolism, and major bleeding compared to those with a sPESI score of 1 or greater. [7]
These findings underscore the potential of the sPESI score in identifying candidates for early hospital discharge or home treatment, offering a promising tool for optimizing patient care. [7]
PESI and sPESI are risk stratification scoring systems used in the medical field to assess the severity and prognosis of patients with pulmonary embolism (PE), a potentially life-threatening condition where a blood clot blocks one of the pulmonary arteries in the lungs.
PESI is a risk assessment tool that helps healthcare providers classify the severity of pulmonary embolism and predict the 30-day mortality rate. It considers various clinical parameters such as age, gender, comorbidities (e.g., heart disease, cancer), vital signs (heart rate, blood pressure), and laboratory values (blood oxygen levels). The PESI score provides a numerical value corresponding to different risk categories, from low risk to high risk.
sPESI is a simplified version of PESI, using fewer variables for easier calculation and clinical use. It includes age, heart rate, systolic blood pressure, and the presence of cancer or chronic lung disease. Like PESI, sPESI categorizes patients into different risk groups based on their scores.
Use of PESI and sPESI:
These scoring systems are primarily used to assist healthcare providers in making informed decisions regarding the management and treatment of patients with pulmonary embolism. The risk stratification provided by PESI or sPESI helps guide decisions about hospitalization, monitoring, and treatment intensity:
These scoring systems provide valuable guidance to healthcare providers in tailoring their approach to each patient's individual risk profile, optimizing patient care and improving outcomes in cases of pulmonary embolism. It's important to note that clinical judgment and individual patient characteristics also play a role in treatment decisions, and these scoring systems are just one component of the overall assessment process.
Pulmonary embolism, PESI, sPESI, risk assessment, severity index, prognosis, calculator, interactive tool, clinical decision-making, treatment guidance, risk stratification, patient care, thrombolytic therapy, outpatient treatment, hospitalization, anticoagulant medications, mortality rate, simplified version, cardiovascular health, medical scoring systems, healthcare, lesson, education.Understanding Pulmonary Embolism Risk Assessment: PESI and sPESI CalculatorsThe PESI & sPESI Scores0000