Integer scores and mortality estimation formulas provided by the Center for Outcomes Research, University of Massachusetts Medical School. [13]
The GRACE score was found in one study to be strongly correlated with the GENSINI score (a coronary artery disease severity index), therefore it is a strong predictor of CAD, particularly in the presence of other risk factors, such as Hypertension, DM, smoking or HFrEF (low ejection fraction Heart Failure). Still, some of these risk factors are not taken into account into the GRACE score calculation but still affect the GENSINI score. The authors note that the GRACE score should still be correlated with clinical status and previous vascular events for further risk stratification. The association between the GRACE score and the GENSINI score was linear. [2]
The GRACE score was also associated with the type of CAD, as patients with low risk scores tended to have healthy coronary atreries or noncritical CAD, while patients with higher scores tended to be affected by three-vessel or left-main artery lesions at a higher rate. [2]
In one study, the GRACE score system was tested against the GUSTO IIb dataset comprising over 12,000 patients, and was found to have excellent discriminatory capacity despite the fact that it didn't account for what the authors note is key prediction parameter. [1] After combining data from 48,389 patients, the validity of the GRACE score was demonstrated by showing that the score had a good correlation with 6-month and 1-year mortality rates for each value, and the discriminatory ability was retained even when patient stratification was done using a simplified GRACE score.
Since the original GRACE study, significant advancements have been made in quantifying seric troponin levels. Ultra-sensitive assays have been developed that can detect this marker at levels over 10 times lower than previous tests, with a sensitivity of over 99% for discovering myocardial ischemic injuries. [10]
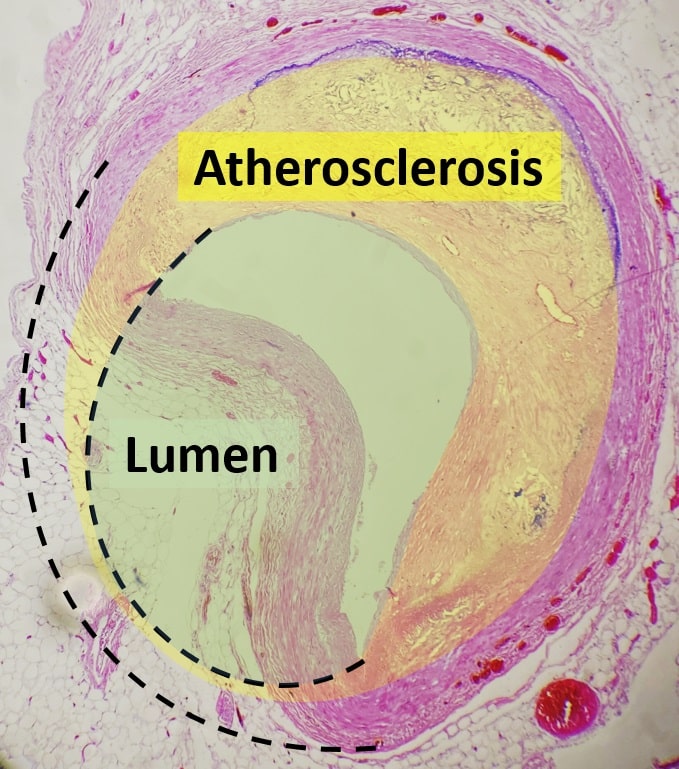
These advancements have improved our understanding of the pathogenesis of MI and the conditions necessary for its occurrence. It was discovered that not all MIs are caused by atherosclerosis, leading to a major update of MI definitions and the identification of two major classes of MI [11]:
It is important to note that even though only a fraction of MI cases (1/10th to 1/3rd) fall into the type 2 category, [11] outcomes for type 2 MI are often poor, with an estimated survival rate of only 30% after 5 years. Interestingly, the rate of additional MI events is similar between the two types. [10]
Although the GRACE score was initially useful in determining mortality in MI patients, further risk stratification was needed, particularly for type 2 MI patients with mixed results. To address this, the new GRACE 2.0 score was developed by incorporating additional risk factors specific to MINOCA patients, allowing for better assessment of mortality risk across all MI population groups.
In a study involving 10,059 patients, the GRACE 2.0 score demonstrated fairly accurate prediction of 1-year mortality rates for MINOCA patients (mainly women), while its accuracy was somewhat lower for CAD-MI patients (predominantly younger, male) [4]. Nevertheless, the updated score showed improved accuracy in identifying high-risk MINOCA patients compared to the original score. It is important to note that both types of patients tended to have underestimated all-cause death according to the GRACE 2.0 score. [10]
Furthermore, for type 1 MI patients, the GRACE 2.0 score exhibited better discrimination for in-hospital death compared to the original GRACE score. [10] The authors acknowledge that the new score was developed before the universal classification for MI, and its applicability to type 2 MI, a heterogeneous condition, may not account for the different parameters required for subgroup stratification even though it was intended for MINOCA patient risk-stratification in mind. Nonetheless, it was demonstrated that all patients with myocardial injury faced an increased cardiovascular risk, with type 2 MI patients having a 4-fold higher risk of further cardiovascular events. The authors suggest that additional studies and risk stratification are necessary for specialized management of each subgroup.
Overall, the GRACE 2.0 score represents an important advancement in risk assessment for myocardial infarction, with a particular focus on type 2 MI patients, and provides valuable insights for improved patient care and outcomes.
The GRACE (Global Registry of Acute Coronary Events) score is a tool used to assess the risk of adverse outcomes in patients with acute coronary syndrome (ACS).
ACS is a term used to describe a range of conditions resulting from reduced blood flow to the heart, such as unstable angina or myocardial infarction (heart attack).
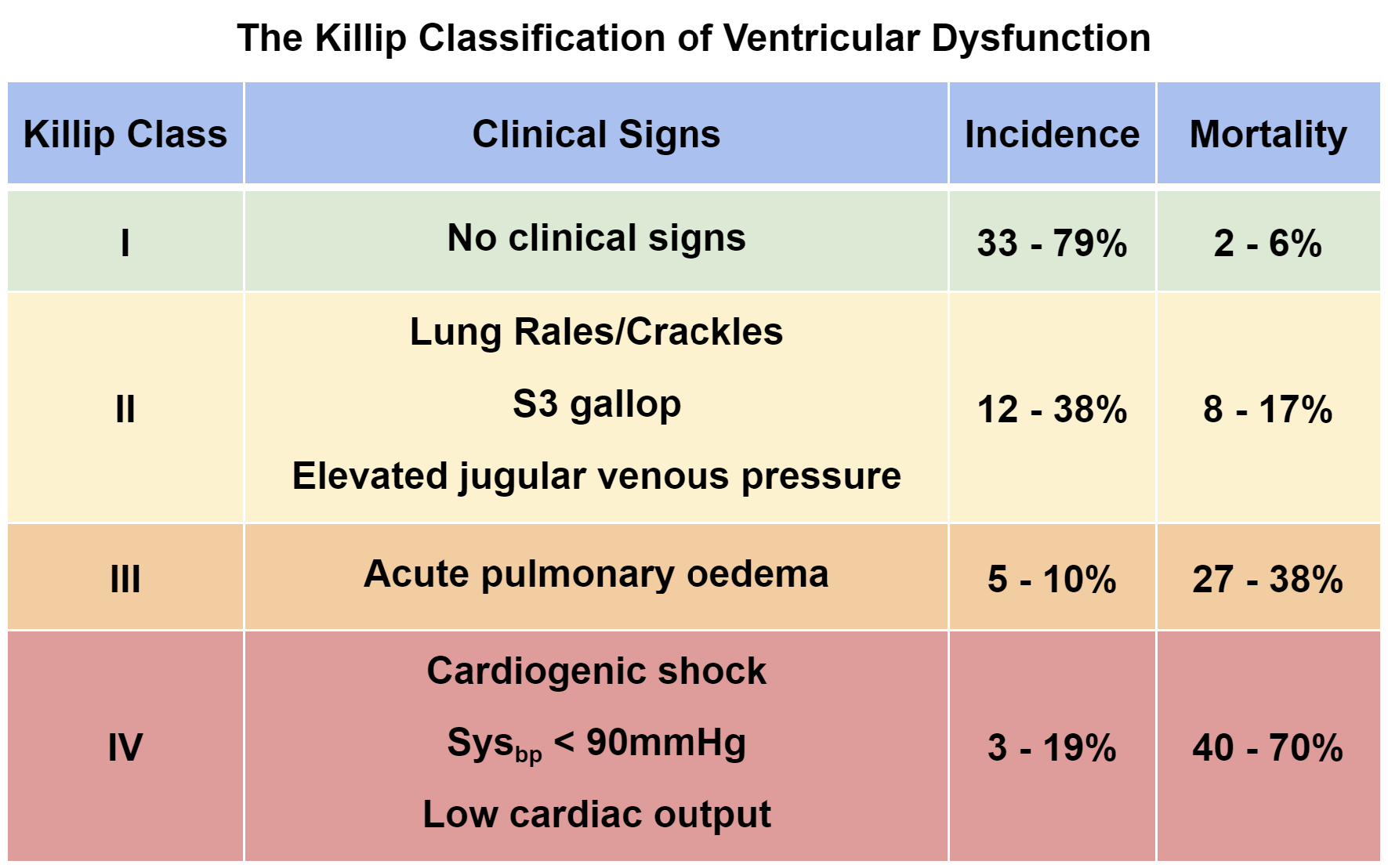
The GRACE score takes into account various clinical factors to estimate the likelihood of death or other serious complications within a specific time frame, typically up to six months. These factors include:
By evaluating these variables, the GRACE score provides a numerical value that reflects the patient's risk profile.
The score is primarily used by healthcare professionals to aid in risk stratification and guide decision-making in the management of ACS patients. It helps clinicians assess the urgency of interventions, determine appropriate treatment strategies, and identify individuals who may benefit from more aggressive interventions or closer monitoring. The GRACE score serves as a tool for risk assessment and can contribute to more personalized and tailored care for patients with ACS.
It's worth noting that medical practices and scoring systems can evolve over time, and there may be newer or alternative risk assessment tools available since my knowledge cutoff in September 2021. It's always a good idea to consult up-to-date medical literature and guidelines or speak with a healthcare professional for the most current and accurate information.
Medical GRACE score calculator, risk assessment, acute coronary syndrome, ACS, clinical factors, age, heart rate, blood pressure, creatinine levels, ECG findings, risk stratification, adverse outcomes, personalized care, patient outcomes, NSTEMI, STEMI, miocardial infarction, atherosclerosis, cardiovascularMastering Risk Assessment: Unveiling the Medical GRACE Score CalculatorThe GRACE score0000