A study conducted on nearly 85,000 patients with STEMI revealed a significant correlation between the TIMI score and mortality. The mortality rate ranged from 1.1% to 30%. Interestingly, the predictive capacity of the score was higher for patients who received acute reperfusion therapy compared to those who did not.[2]
For NSTEMI patients, the TIMI score also exhibited a strong correlation with mortality rates within 30 days. The mortality rate ranged from 2.1% for a score of 0 up to 100% for a score of 7, as observed in a study involving 3,929 patients[3]. Among this group, hypertension and active tobacco use were noted as the most frequent cardiac risk factors. It is worth noting that the majority of patients in the study were under 65 years old, and only one patient had a TIMI score of 7, which may limit the generalizability of the results and the representativeness of the population.[2]
The GRACE scores demonstrated better discriminatory ability compared to the TIMI UA/NSTEMI score when predicting in-hospital and 6-month mortality in patients with unstable angina (UA) or non-ST-segment elevation myocardial infarction (NSTEMI). However, both the GRACE and TIMI STEMI scores performed equally well in predicting outcomes for patients with ST-segment elevation myocardial infarction (STEMI). The observed difference in discriminative ability is likely due to the exclusion of essential risk factors in the first score.[4]
In other words, it is best suited to use the GRACE score for NSTEMI patients, and any of the two scores for STEMI cases. Howerver, the new Dyanmic TIMI score might be better suited for STEMI patients than the original version.[4]
In another study involving 3,451 patients, it was found that the TIMI score might also be well suited for estimating mortality at 1 year after hospital discharge. A meta-analysis highlighted that the correlation extended not only to the factors measured in the TIMI score for 1-year mortality, but also with stroke, renal failure, congestive heart failure (CHF)/shock, major bleeds, and arrhythmias, in that order. [5]
The same meta-analysis identified some protective factors, although their influence on outcomes was relatively weaker compared to the risk factors. These protective factors included coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI), and urgent revascularization. However, it is important to note that the confidence intervals for these findings were not as strong. Additionally, the meta-analysis team developed a new score called "The Dynamic TIMI RISK SCORE" for better prediction of patient outcomes. It is essential to mention that this new score was specifically verified for use in STEMI patients. [5]
Furthermore, the TIMI score is not only valuable during the initial presentation but can also be used for risk assessment over time. Serial TIMI score measurements enable monitoring of a patient's response to treatment and guide subsequent management decisions.
The Dynamic TIMI (Thrombolysis in Myocardial Infarction) Score is an enhanced version of the traditional TIMI score specifically designed for risk assessment and outcome prediction in patients with ST-segment elevation myocardial infarction (STEMI). It incorporates additional factors and has been developed to improve the accuracy and optimization of cardiovascular risk calculation for STEMI patients.
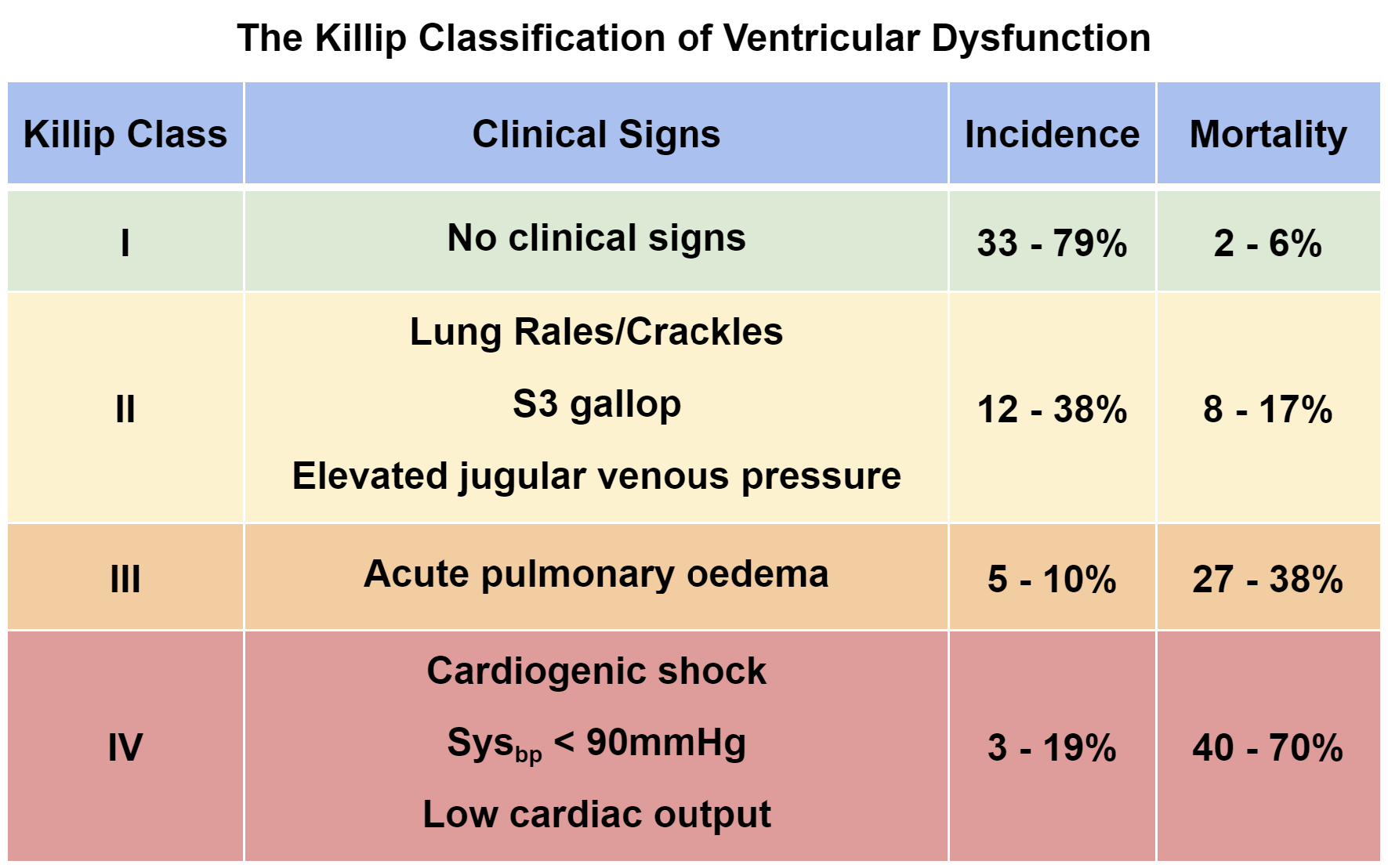
The Dynamic TIMI score takes into account various clinical variables such as age, heart rate, systolic blood pressure, Killip class (a measure of heart failure severity), and biomarkers like cardiac troponin. By considering these factors, the Dynamic TIMI score provides a comprehensive assessment of the patient's risk profile, allowing clinicians to better predict outcomes and tailor treatment strategies accordingly.
This updated scoring system aims to provide a more nuanced evaluation of STEMI patients, taking into consideration both traditional risk factors and emerging prognostic markers. By incorporating these additional factors, the Dynamic TIMI score enhances risk stratification and assists clinicians in making informed decisions regarding reperfusion therapies, invasive procedures, and other management strategies.
The use of the Dynamic TIMI score facilitates more personalized and targeted care for STEMI patients, enabling healthcare professionals to identify individuals who are at higher risk for adverse cardiovascular events. This allows for more aggressive interventions and closer monitoring in high-risk patients, while potentially sparing lower-risk patients from unnecessary procedures.
It is important to note that the Dynamic TIMI score is specifically validated and recommended for use in STEMI patients. Its application in other cardiac conditions or patient populations may not be as reliable or accurate. As with any scoring system, clinical judgment should also be exercised, and individual patient characteristics and comorbidities should be considered in conjunction with the Dynamic TIMI score for optimal risk assessment and management.
Dynamic TIMI score calculator, cardiovascular risk, acute coronary syndromes, ACS, risk assessment, treatment decisions, risk categorization, factors, implementation, clinical practice, prognosis evaluation, STEMI, Cardiology, Vascular, AtherosclerosisThe Dynamic TIMI Score Calculator: Enhancing Cardiovascular Risk Assessment for STEMI PatientsThe Dynamic TIMI Score for STEMI0000