The original CHADS and CHADS-VASC scores demonstrate a significant correlation with the risk of developing stroke in patients with atrial fibrillation (AF), and have been included in the European Society of Cardiology (ESC) guidelines for the management and surveillance of AF patients. [1]
In a study involving over 100,000 patients:
The incidence rate of ICH was 0.6 per 100 person-years, while major bleeding events occurred at a rate of 2.3 per 100 person-years of life [3].
Anti-thrombotic therapy did not influence the frequency of ICH or major bleeding. Other factors, such as female gender, myocardial infarction, vascular disease, diabetes, obesity, thyroid disease, and accidental falls, were also studied and did not show a significant influence on bleeding frequency [3].
Studies have indicated that each 1-point increase in the original CHADS2 score is associated with a 1.5 increase in the rate of stroke per 100 patient-years [2]. Furthermore, the new score has demonstrated an even stronger correlation with stroke risk in multiple studies [1][4].
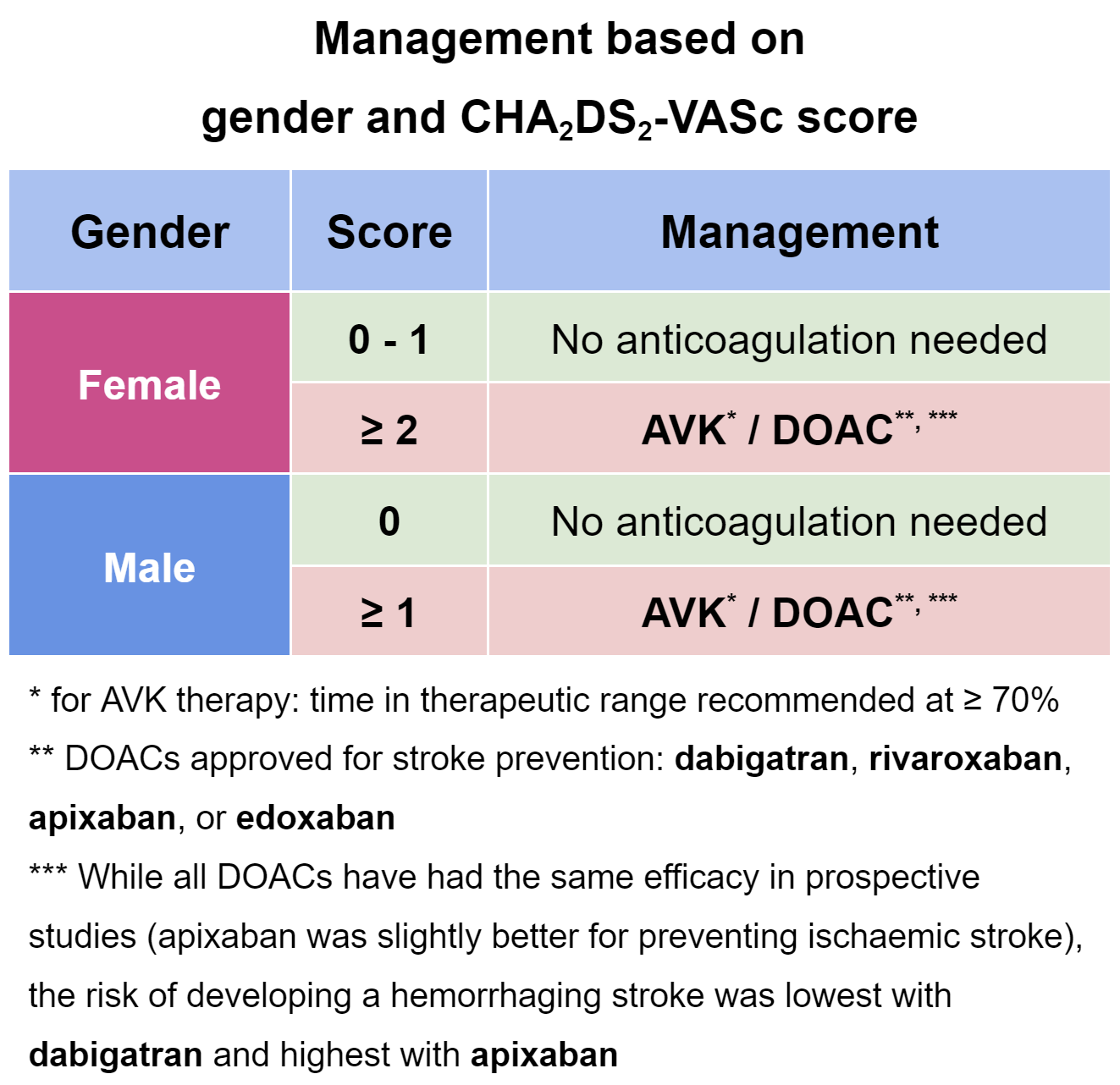
According to a study, the overall ischemic stroke rate in non-anticoagulated AF patients was 3.20 per 100 person-years. The rates of thromboembolic events varied significantly based on conflicting treatment thresholds between European and U.S. guidelines. The European guideline recommends oral anticoagulant treatment for males with a CHA2DS2-VASc score of 1 or females with a score of 2, while the U.S. guideline offers a Class IIb recommendation for no treatment, aspirin therapy, or oral anticoagulant treatment for AF patients with a CHA2DS2-VASc score of 1 [3].
A study has shown that patients with heart failure and high CHADS-VASC scores tend to develop atrial fibrillation sooner [5]. This study also reported a slightly higher mortality rate, although the difference was statistically significant but not particularly large. Nonetheless, the study suggests that CHADS-VASC scores can serve as a useful tool not only for managing AF patients but also for predicting the probability of developing AF in selected patients, though further investigation is warranted [5].
The CHA₂DS₂-VASc score is a widely used clinical tool for assessing the risk of stroke in patients with atrial fibrillation (AF). It helps healthcare professionals determine the need for anticoagulation therapy to prevent thromboembolic events such as stroke.
The acronym "CHA₂DS₂-VASc" stands for the different risk factors included in the scoring system:
Each risk factor is assigned a certain number of points based on its significance in predicting stroke risk. By summing up the points corresponding to the patient's risk factors, a numerical CHA₂DS₂-VASc score is obtained. The higher the score, the higher the stroke risk.
The CHA₂DS₂-VASc score assists healthcare providers in stratifying patients into different risk categories, guiding treatment decisions regarding the initiation of anticoagulation therapy. It helps ensure that patients at higher risk of stroke receive appropriate preventive measures, while those at lower risk can avoid unnecessary medication.
Overall, the CHA₂DS₂-VASc score plays a crucial role in optimizing stroke prevention strategies for individuals with atrial fibrillation, ultimately contributing to better patient outcomes.
Stroke risk assessment, CHA2DS2-VASc score, Atrial fibrillation (AF), Risk stratification, Clinical implications, Calculator, Patient characteristics, Thromboembolic events, Anticoagulation therapy, Stroke prevention, CHA2DS2-VASc score calculator, Stroke risk calculator, Atrial fibrillation risk assessment tool, Thromboembolic risk calculator, Clinical decision support tool, Risk stratification tool, Patient-specific stroke risk score, Anticoagulation therapy recommendation, Individualized treatment approach, Stroke prevention calculatorAssessing Stroke Risk: Understanding and Using the CHA₂DS₂-VASc ScoreThe CHA2DS2–VASc score0000