In one study[7] that admitted 399 patients that presented to the emergency department for upper G.I. bleed (age >16 years), only 19 patients rebled (4.76%), and the most common causes for re-bleeding were:
Only 26 (6.52%) patients died within 30 days of presentation. In that study, no patients that were attributed a Glasgow-Blatchford score of less than 3 re-bled or died within the first 30 days from admission, so these patients could be considered suitable for discharge. Still, the authors note that a low G-B score does not exclude the need for a diagnostic Oesophago-Gastro-Duodenoscopy, so always plan further outpatient specialty investigations.[7]
The Glagow-Blatchford scoring system is a tool used to predict the risk of death or major bleeding in patients with upper gastrointestinal bleeding. It was developed in 2000 by a team led by Dr. Oliver Blatchford and is based on a combination of clinical, laboratory, and endoscopic factors.
The score ranges from 0 to 23, with higher scores indicating a higher risk of adverse outcomes. The system is widely used in clinical practice and has been validated in multiple studies. It can be used to guide management decisions, such as the need for admission to an intensive care unit, blood transfusion, and endoscopic intervention.
The Blatchford scoring system is a clinical prediction rule that uses a combination of 9 easily obtainable clinical, laboratory and endoscopic parameters to predict the risk of death or need for surgery in patients with upper gastrointestinal bleeding.
These parameters include: initial systolic blood pressure, heart rate, presence of comorbidities (such as cirrhosis or cardiac failure), hemoglobin level, serum urea level/BUN and presence of melena (black, tarry stools). Each of these parameters is assigned a certain number of points, and the total score ranges from 0 to 23, with higher scores indicating a higher risk of adverse outcomes.
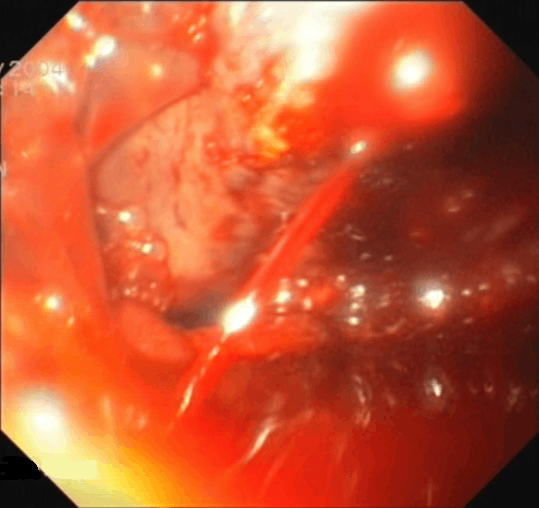
These parameters can also be correlated with the presence of hematemesis (vomiting of blood), presence of shock, and endoscopic stigmata of recent bleeding, and there are other risk-measuring scores like the AIMS65 or the Rockall score that also include these other factors.
The system has been validated in multiple studies, and has been shown to have good predictive accuracy in different populations and settings. It has been shown to be useful in identifying patients who are at low risk of adverse outcomes and can be safely discharged, as well as those who are at high risk and require more aggressive management such as intensive care unit admission, blood transfusion, and endoscopic intervention.
It is important to note that the Blatchford scoring system is not intended to replace clinical judgment, but rather to provide a standardized tool that can be used to guide decision making in patients with upper gastrointestinal bleeding.
score, calculator, Glasgow, Blatchford, bleeding, GIT, hemorrhage, haemorrhage, hemoglobin, 2001, 2000, gastric, gastro, intestnal, gastrointestinal, tract, UGIBThe Glasgow-Blatchford upper gastrointestinal bleeding score calculatorBlatchford score calculator0000